🩺 Cervical Cancer: Complete Patient Guide
A comprehensive, patient-friendly guide to cervical cancer — causes, symptoms, diagnosis, staging, treatment, prevention, and recovery. Learn how HPV infection leads to cervical cancer, understand your treatment options, and find answers to common patient questions.
🌸 Overview: Understanding Cervical Cancer
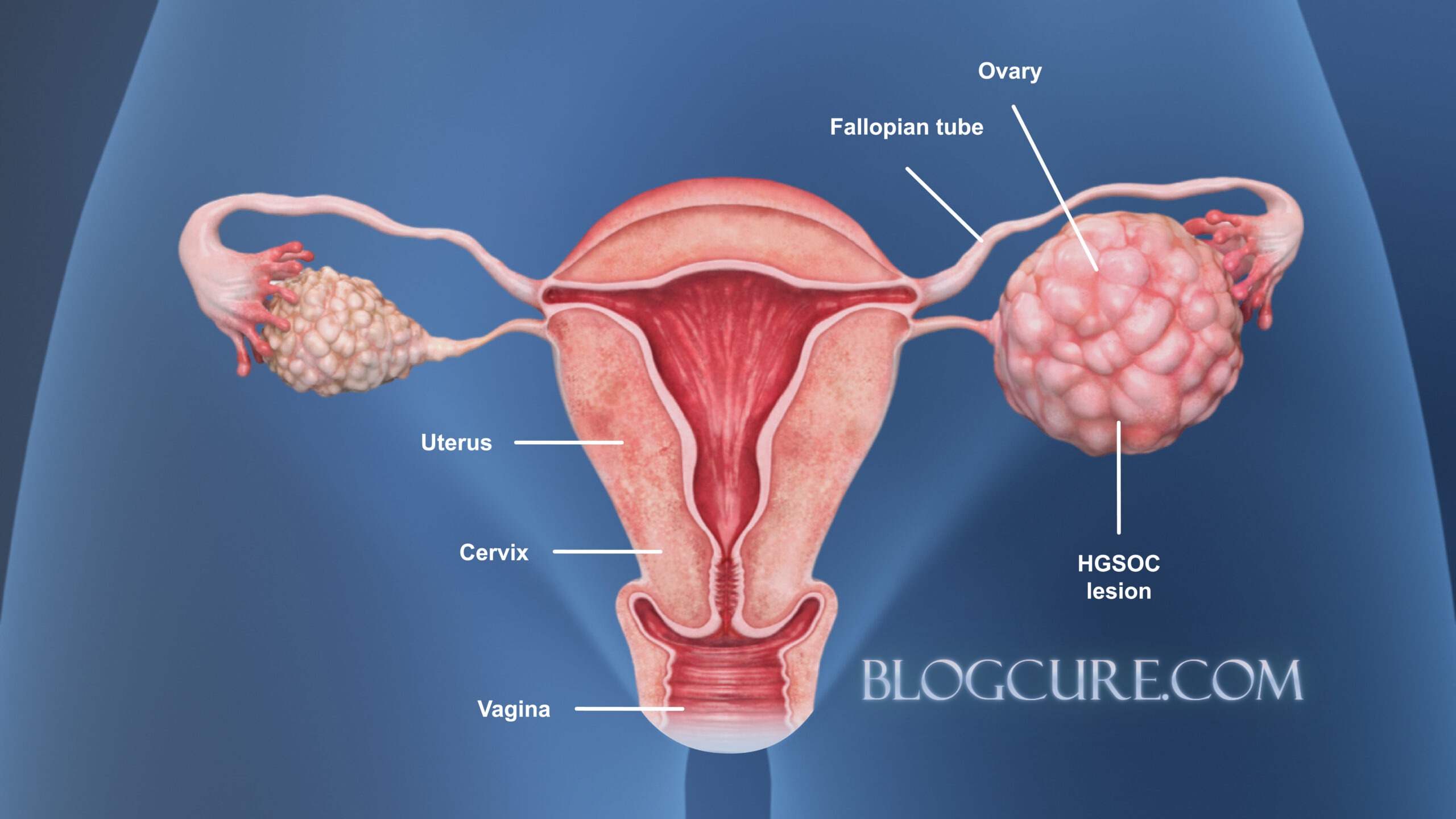
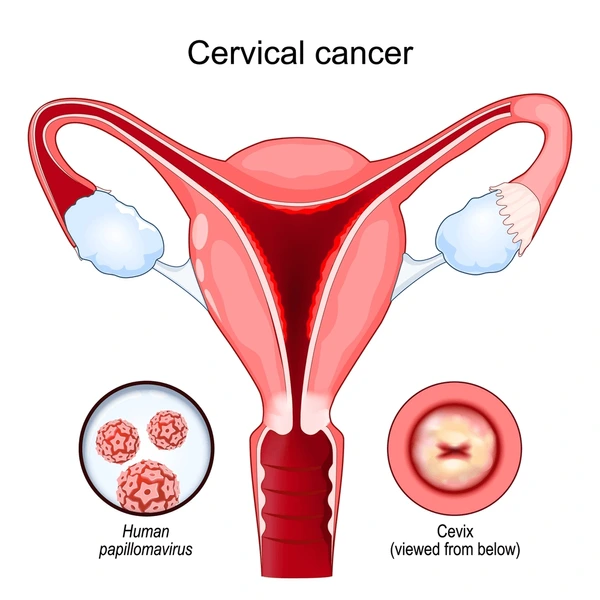
Cervical cancer develops in the cervix — the lower part of the uterus that connects to the vagina. Once among the leading causes of cancer-related deaths in women, its rate has dramatically decreased with routine Pap and HPV screening.
In 2018, an estimated 2,500 women in Türkiye were diagnosed with cervical cancer, and around 1,250 died from the disease. When detected early, the 5-year survival rate exceeds 90%.
Cervical cancer mainly affects women aged 30–50, although it can occur after menopause. It ranks as the third most common cancer among women under 40.
There are two major types:
| Type | Origin | Description |
|---|---|---|
| Squamous Cell Carcinoma | Outer surface of the cervix | The most common form; starts in the squamous epithelial cells. |
| Adenocarcinoma | Cervical canal glands | Less common; harder to detect through standard screening. |
🧬 What Causes Cervical Cancer?
The primary cause of cervical cancer is persistent infection with high-risk types of Human Papillomavirus (HPV) — a common sexually transmitted virus.
Nearly 80% of sexually active women encounter HPV during their lifetime, but only a small portion develop cancer.
High-risk HPV types:
| HPV Type | Risk Level | Notes |
|---|---|---|
| 16 | Very high | Responsible for ~60% of cervical cancers |
| 18 | High | Found in ~15% of cases |
| Others (31, 33, 45, 52, 58) | Moderate | May also cause cancer |
Not every HPV infection leads to cancer. In most cases, the immune system clears the virus within two years. However, long-term infection with high-risk types may cause abnormal cell growth, leading to precancerous lesions (CIN — Cervical Intraepithelial Neoplasia) that can progress to cancer over several years.
⚠️ Risk Factors for Cervical Cancer

Certain conditions increase the risk of developing cervical cancer:
- 🌿 Early sexual activity (before age 16)
- ❤️ Multiple sexual partners or a partner with multiple partners
- 🚬 Smoking
- 🧫 Weakened immune system (HIV, organ transplant, long-term steroids)
- 💊 Long-term use of birth control pills (over 5 years)
- 🍔 Poor diet low in fruits and vegetables
- 🤰 High number of pregnancies
- 💉 Not receiving HPV vaccination
- 🩸 Previous abnormal Pap smear or untreated precancerous lesions
💡 Symptoms and Early Warning Signs

Cervical cancer often has no symptoms in its early stages, which is why regular screening is critical.
As it progresses, the following symptoms may appear:
- 💔 Vaginal bleeding after intercourse
- 🩸 Irregular bleeding between periods
- 🌙 Postmenopausal bleeding
- 💧 Watery, foul-smelling vaginal discharge
- ⚡ Pelvic or back pain
- 🦵 Swelling in the legs
- 🍽️ Loss of appetite and unexplained weight loss
- 😴 Fatigue or weakness
Tip: Any vaginal bleeding after menopause or after sex should always be checked by a gynecologist.
🔍 Diagnosis and Screening
Early detection is the key to preventing invasive cervical cancer. The two main screening methods are:
| Test | Purpose | Frequency |
|---|---|---|
| Pap Smear (Pap Test) | Detects abnormal cervical cells | Every 3 years (ages 21–65) |
| HPV Test | Detects high-risk HPV infection | Every 5 years (ages 30–65) |
How it works:
A small sample of cervical cells is collected using a soft brush or spatula. The procedure is quick, safe, and usually painless.
If results are abnormal, your doctor may perform colposcopy — a magnified examination of the cervix with special solutions — and may take a biopsy for laboratory analysis.
🩻 Staging of Cervical Cancer
Staging determines how far the cancer has spread and guides treatment decisions.
| Stage | Description |
|---|---|
| Stage I | Cancer confined to the cervix |
| Stage II | Spread to nearby tissues or upper vagina |
| Stage III | Spread to pelvic wall or lymph nodes |
| Stage IV | Spread to bladder, rectum, or distant organs like liver or lungs |
💊 Treatment Options
Treatment depends on the stage of cancer, patient’s age, overall health, and fertility wishes.
1️⃣ Surgical Treatments
🩺 Early-stage cervical cancer may be treated surgically:
- Conization: Removal of a cone-shaped portion of the cervix (for very early lesions).
- Simple Hysterectomy: Removal of the uterus and cervix.
- Radical Hysterectomy: Removal of uterus, cervix, nearby tissues, and part of the vagina.
- Radical Trachelectomy: Removes the cervix but preserves the uterus — suitable for women wishing to preserve fertility.
- Lymph Node Dissection: Checks for cancer spread.
2️⃣ Radiation Therapy (R/T)
Uses high-energy X-rays to kill cancer cells. It can be external (from a machine) or internal (brachytherapy).
3️⃣ Chemotherapy (C/T)
Uses drugs to destroy cancer cells throughout the body.
Common medication: Cisplatin, often combined with radiation (chemoradiation) to boost effectiveness.
| Stage | Recommended Treatment | Fertility Preservation |
|---|---|---|
| Early I | Surgery (Trachelectomy or Hysterectomy) | Possible |
| II–III | Chemoradiation | Not possible |
| IV | Palliative chemo/radiation | Not possible |
🌿 Post-Treatment Follow-Up
After treatment, regular follow-up visits are essential to monitor recovery and detect any recurrence.
| Time Period | Frequency of Check-ups |
|---|---|
| First 2 years | Every 3–4 months |
| Years 3–5 | Every 6 months |
| After 5 years | Once a year |
These visits may include:
- Pelvic exam and Pap test
- Imaging (ultrasound, CT, or MRI) if symptoms appear
- Counseling for sexual health and emotional well-being
💉 HPV Vaccine: Prevention is Better Than Cure
HPV vaccination is the most effective way to prevent cervical cancer.
| Age Group | Doses | Notes |
|---|---|---|
| 9–15 years | 2 doses | Ideal time for vaccination |
| 16–26 years | 3 doses | Catch-up vaccination |
| >26 years | Optional | May still offer protection |
Other preventive measures:
- ✅ Regular Pap or HPV screening
- ✅ Practice safe sex (condom use)
- ✅ Avoid smoking
- ✅ Maintain a healthy diet rich in fruits and vegetables
- ✅ Limit the number of sexual partners
📊 Cervical Cancer at a Glance
| Fact | Statistic |
|---|---|
| 5-year survival (early stage) | >90% |
| Age group most affected | 30–50 years |
| Global cause | Persistent high-risk HPV infection |
| Preventable through vaccination | Yes |
| Curable if detected early | Yes |
❓ Frequently Asked Questions (FAQ)
1️⃣ What is the main cause of cervical cancer?
Persistent infection with high-risk HPV types (especially HPV-16 and 18).
2️⃣ Can cervical cancer be cured?
Yes, when detected and treated early, cervical cancer is almost 100% curable.
3️⃣ Is cervical cancer contagious?
No, but HPV, the virus causing it, is transmitted sexually.
4️⃣ Can I get cervical cancer even if I have no symptoms?
Yes — early stages are asymptomatic, making regular screening vital.
5️⃣ What are early signs I should watch for?
Unusual vaginal bleeding, discharge, pelvic pain, or pain after sex.
6️⃣ How often should I get a Pap or HPV test?
Pap test every 3 years (ages 21–65) or HPV test every 5 years (ages 30–65).
7️⃣ Does HPV vaccine eliminate all risk?
It prevents most high-risk HPV types, but screening should continue.
8️⃣ Can I have children after treatment?
In early stages, fertility-sparing surgeries like trachelectomy may be possible.
9️⃣ What if my test results are abnormal?
Your doctor may recommend colposcopy and biopsy for confirmation.
🔟 How can I lower my risk naturally?
Quit smoking, practice safe sex, maintain a strong immune system, and eat healthily.
11️⃣ Is cervical cancer painful?
Usually not in early stages; advanced cases may cause back or pelvic pain.
12️⃣ How soon should I see a gynecologic oncologist?
Immediately if abnormal test results or symptoms appear.