🩺
🌸 Introduction
Uterine fibroids and ovarian cysts are two of the most common gynecological conditions affecting women of reproductive age. While both are usually benign (non-cancerous), they can lead to discomfort, pain, or fertility issues if not properly diagnosed and managed.
Understanding these conditions helps women make informed decisions about their health, recognize early symptoms, and seek timely treatment.
In this comprehensive guide, we’ll cover everything you need to know — from causes and risk factors to diagnosis, treatment, and lifestyle advice.
🔹 What Are Uterine Fibroids (Myomas)?

Uterine fibroids, also called myomas or leiomyomas, are non-cancerous growths that develop from the smooth muscle tissue of the uterus (womb).
They can appear as a single mass or as multiple clusters and vary in size — from a tiny seed to a bulky mass that distorts the uterus.
🧬 Key Facts
- Benign (non-cancerous) smooth muscle tumors
- Common during reproductive years (ages 30–45)
- Can grow inside, within, or outside the uterine wall
- Influenced by hormones, genetics, and lifestyle factors
📊 Table: Common Risk Factors for Fibroids
| Risk Factor | Description | Influence |
|---|---|---|
| Hormonal imbalance | High levels of estrogen and progesterone | Stimulates fibroid growth |
| Genetics | Family history of fibroids | Increases risk 2–3 times |
| Obesity | High body fat raises estrogen levels | Increases likelihood of fibroid development |
| Early menarche | First menstruation before age 11 | Linked to higher fibroid risk |
| Red meat consumption | Diet rich in red meat and low in vegetables | Associated with fibroid formation |
| Alcohol & caffeine | Excessive intake | Can disrupt hormonal balance |
💢 Symptoms of Uterine Fibroids

Many women with fibroids experience no symptoms, but when symptoms occur, they depend on the size, number, and location of the fibroids.
Common Symptoms
- 🩸 Heavy or prolonged menstrual bleeding
- 🔁 Irregular periods or spotting between cycles
- ⚡ Pelvic or lower back pain
- 🌕 Abdominal swelling or pressure
- 💔 Pain during sexual intercourse
- 🚻 Frequent urination or constipation
- 🤰 Difficulty conceiving or maintaining pregnancy
🧠 Table: Fibroid Symptoms and Related Systems
| Symptom | Affected Area | Possible Cause |
|---|---|---|
| Heavy bleeding | Uterine lining | Submucosal fibroid |
| Abdominal pain | Pelvic muscles | Large or multiple fibroids |
| Urination issues | Bladder | Fibroid pressing on bladder |
| Constipation | Colon | Posterior uterine fibroid |
| Infertility | Reproductive tract | Blocked tubes or uterine distortion |
🧩 Diagnosis: How Are Fibroids Detected?
Fibroids are often found during routine gynecological exams. However, imaging tests provide more accurate information about their size, number, and location.
Diagnostic Methods
- 🩺 Pelvic Examination — Doctor feels the uterus for irregularities.
- 🖥️ Ultrasound (USG) — Uses sound waves to visualize fibroids and determine size/location.
- 🧲 Magnetic Resonance Imaging (MRI) — Gives detailed soft-tissue images; best for large or complex cases.
- 🔍 Hysteroscopy — A small camera inserted through the vagina to inspect the uterus directly.
- 💉 Blood Tests — To check for anemia due to heavy bleeding.
⚕️ Treatment Options for Uterine Fibroids
The choice of treatment for uterine fibroids depends on several factors — such as age, symptoms, fertility plans, and the size or location of the fibroids.
While some fibroids require only regular monitoring, others may need medical or surgical treatment.
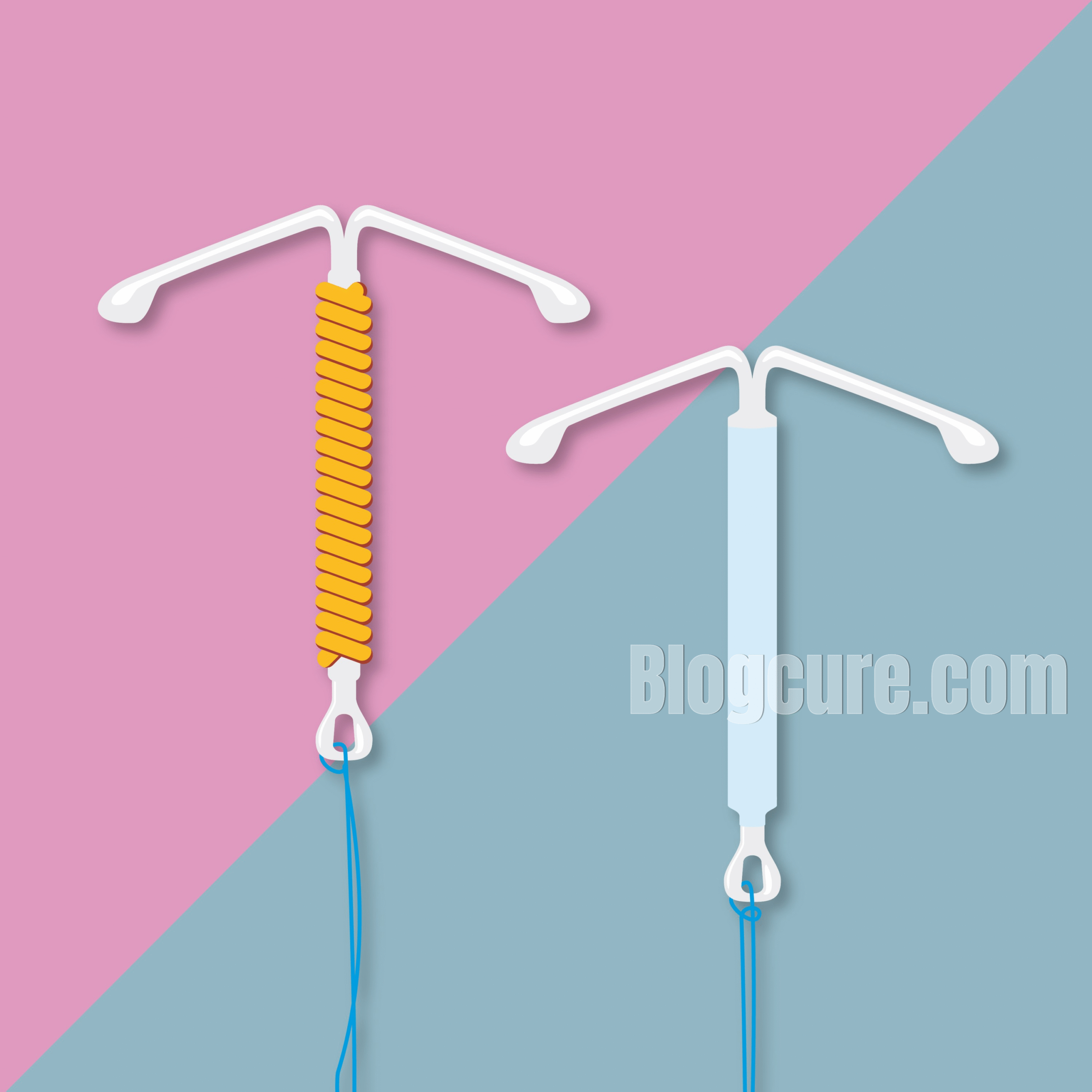
💊 1️⃣ Medical (Non-Surgical) Treatments
Medical treatments focus on managing symptoms such as heavy bleeding, pain, and hormonal imbalance rather than completely removing fibroids.
| Treatment Type | Example | Purpose |
|---|---|---|
| Hormonal Therapy | Birth control pills, GnRH agonists | Controls heavy bleeding and reduces fibroid size |
| Progestin IUD (Intrauterine Device) | Mirena® or similar | Reduces bleeding without shrinking fibroids |
| Tranexamic Acid | Oral medication | Helps prevent excessive menstrual bleeding |
| Iron Supplements | Ferrous sulfate | Manages anemia caused by blood loss |
💡 Tip: Medications can temporarily shrink fibroids, but once discontinued, fibroids may grow back. Regular follow-up is essential.
🏥 2️⃣ Surgical Treatments
When fibroids cause severe symptoms or infertility, surgery may be recommended.
There are multiple options depending on whether you wish to preserve your uterus.
✂️ Myomectomy (Fibroid Removal)
- Best for women who want to keep their uterus and fertility.
- Removes fibroids while leaving the uterus intact.
- Can be done laparoscopically (keyhole) or open surgery depending on fibroid size.
- 💕 Recovery time: 2–6 weeks.
🩻 Hysterectomy (Uterus Removal)
- Removes the entire uterus, and in some cases, the cervix.
- Suitable for women who have completed childbearing.
- Prevents recurrence of fibroids.
- 💕 Recovery time: 4–8 weeks.
🔭 Hysteroscopic Myomectomy
- Minimally invasive procedure performed via the vaginal route.
- Ideal for submucosal fibroids that cause bleeding.
- 💕 Recovery time: 1–2 days.
🤖 Laparoscopic / Robotic Surgery
- Advanced minimally invasive techniques.
- Smaller incisions, less bleeding, quicker healing.
- Best for fibroids under 10 cm.
💉 3️⃣ Uterine Fibroid Embolization (UFE) — Non-Surgical Option
UFE (also known as uterine artery embolization) is a modern, minimally invasive technique used to shrink fibroids by blocking their blood supply.
It’s performed by interventional radiologists under local anesthesia — no large incision, no uterus removal.
🧬 Procedure Overview
- Patient lies on an angiography table.
- Local anesthesia is applied to the groin area.
- A thin catheter is inserted into the femoral artery.
- Tiny particles are injected to block the arteries feeding the fibroids.
- Once the blood supply is cut off, fibroids shrink over time.
💕 Benefits
- No general anesthesia
- No major surgery
- Short hospital stay (usually 1 night)
- Uterus preservation
- Quick recovery (about 7–10 days)
⚠️ Possible Side Effects
- Cramping or pelvic pain for a few days
- Low-grade fever
- Nausea or fatigue during recovery
🩸 Table: Comparison of Fibroid Treatment Methods
| Method | Invasiveness | Recovery | Fertility Preservation | Hospital Stay |
|---|---|---|---|---|
| Medication | None | Minimal | ✅ Preserved | Outpatient |
| Myomectomy | Surgical | 2–6 weeks | ✅ Preserved | 1–2 days |
| Hysterectomy | Major surgery | 4–8 weeks | ❌ Lost | 3–5 days |
| UFE (Embolization) | Minimally invasive | 7–10 days | ✅ Preserved | 1 night |
| Hysteroscopy | Minimally invasive | 1–2 days | ✅ Preserved | Outpatient |
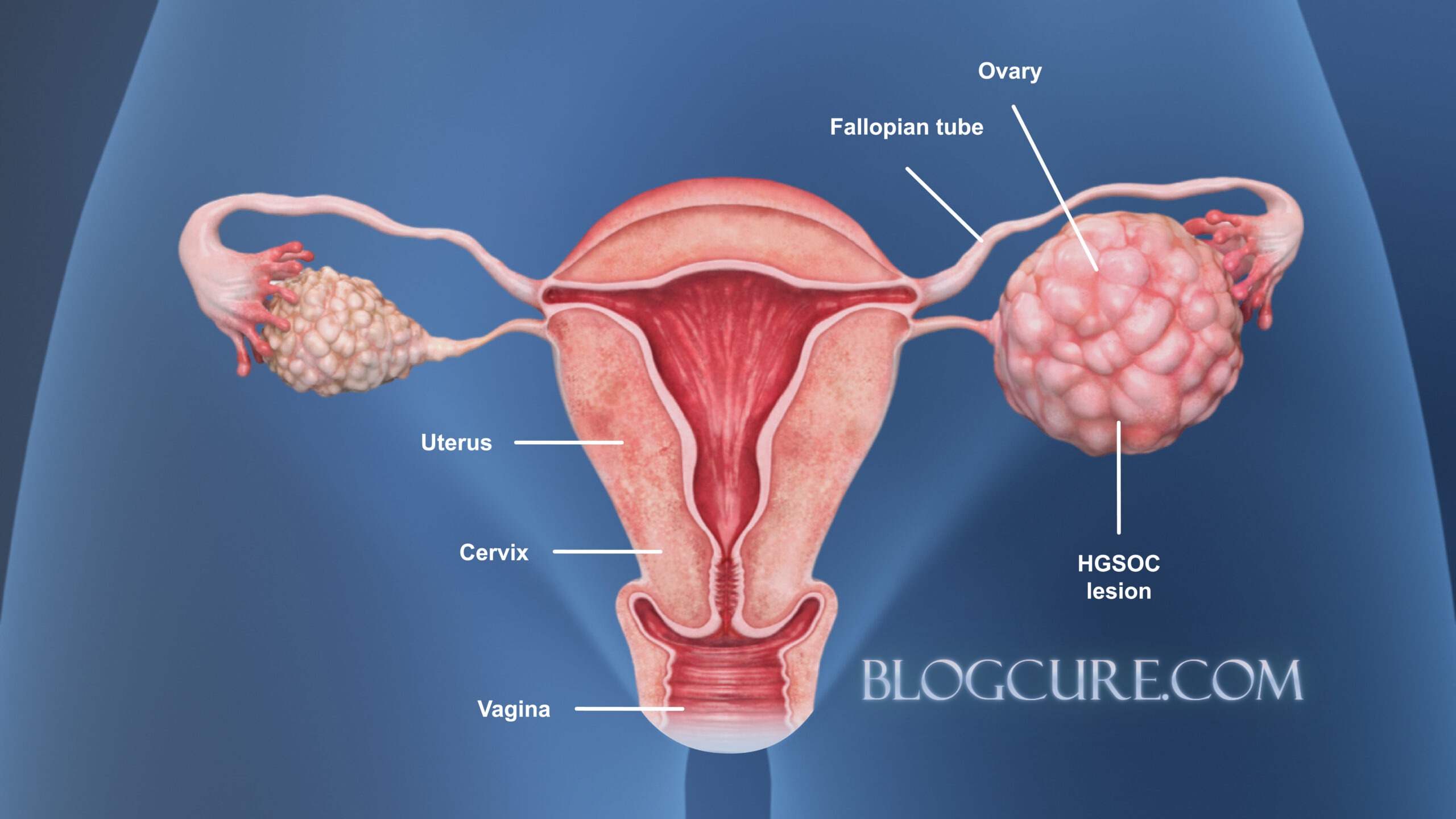
🌺 What Are Ovarian Cysts?
Ovarian cysts are fluid-filled sacs that develop on or inside the ovaries.
Most are benign and resolve spontaneously, but some can cause pain, hormonal changes, or complications like torsion or rupture.
🔬 Types of Ovarian Cysts
| Type | Description | Risk / Concern |
|---|---|---|
| Functional cysts | Form during normal ovulation | Usually harmless, disappear naturally |
| Dermoid cysts | Contain hair, fat, or tissue (congenital) | Can grow large, require surgery |
| Endometriomas (“chocolate cysts”) | Caused by endometriosis | May cause infertility and chronic pain |
| Hemorrhagic cysts | Blood-filled cysts | May rupture and cause severe pain |
| Polycystic ovaries (PCOS) | Multiple small cysts due to hormonal imbalance | Linked to irregular cycles and infertility |
⚠️ Common Symptoms of Ovarian Cysts
- 🌡️ Lower abdominal or pelvic pain
- 🔁 Irregular menstrual cycles
- 🩸 Spotting or heavy bleeding
- 😣 Pain during intercourse
- 🚻 Frequent urination or bloating
- ⚡ Sudden severe pain (possible rupture or torsion)
🩺 Diagnosis of Ovarian Cysts
Diagnosis often involves a combination of clinical evaluation and imaging techniques:
- 🖥️ Ultrasound — First-line method to detect cysts and measure size.
- 🧲 MRI or CT Scan — Used when cysts are large or complex.
- 💉 Blood Tests (CA-125) — Helps differentiate between benign and malignant cysts.
- 🩸 Hormone Tests — Evaluate for PCOS or hormonal imbalance.
- 🔍 Laparoscopy — Both diagnostic and therapeutic in select cases.
💊 Treatment for Ovarian Cysts
Most ovarian cysts are harmless and disappear on their own, but some may need medical attention — especially if they cause pain, grow in size, or have atypical imaging features.
🧩 Treatment Options
| Treatment Type | Description | Best For | Notes |
|---|---|---|---|
| Watchful Waiting | Monitoring cyst size and symptoms over several menstrual cycles | Functional or small cysts | Regular ultrasound follow-up is essential |
| Medication | Birth control pills or hormonal therapy | Hormonal imbalance or recurrent cysts | Helps regulate ovulation and prevent new cysts |
| Laparoscopy | Minimally invasive surgery using small incisions | Persistent or painful cysts | Short recovery, minimal scarring |
| Laparotomy | Open surgery for large or suspicious cysts | Complex or cancerous cysts | Requires general anesthesia |
| Emergency Surgery | For torsion (twisting) or rupture | Acute severe pain | Immediate medical attention needed |
⚕️ Post-Treatment Care
- Rest and hydration 🧘♀️
- Avoid heavy lifting for a few days 🛑
- Follow-up ultrasound after 6–8 weeks 🩺
- Inform your doctor if you experience fever, persistent pain, or abnormal bleeding
🌿 Lifestyle & Prevention Tips
Maintaining a healthy lifestyle can help reduce the risk of fibroids and cysts or prevent recurrence after treatment.
🩷 Key Recommendations
| Tip | Description |
|---|---|
| 🍎 Eat a balanced diet | Focus on fruits, vegetables, whole grains, and fiber. Limit red meat and processed foods. |
| ⚖️ Maintain a healthy weight | Obesity increases estrogen levels, promoting fibroid and cyst growth. |
| 🧘♀️ Manage stress | Chronic stress can disrupt hormone balance. Try yoga or meditation. |
| 🚶♀️ Exercise regularly | At least 30 minutes of moderate activity daily improves circulation and hormone regulation. |
| 🚭 Avoid smoking & limit alcohol | Both can worsen hormonal imbalance and increase risk of gynecological disorders. |
| 👩⚕️ Schedule regular gynecological check-ups | Early detection ensures better outcomes and prevents complications. |
❓ Frequently Asked Questions (FAQ)

1️⃣ What causes uterine fibroids to develop?
Fibroids develop due to a combination of hormonal, genetic, and environmental factors. High levels of estrogen and progesterone stimulate uterine muscle growth.
Risk factors include family history, obesity, early menstruation, and red meat–rich diets. Women aged 30–45 are most commonly affected.
💡 Tip: Fibroids often shrink after menopause because hormone levels decrease.
2️⃣ Can fibroids turn into cancer?
🩺 Very rarely. Less than 1 in 1,000 fibroids becomes malignant (a condition called leiomyosarcoma).
However, rapidly growing fibroids or those that continue to enlarge after menopause require careful evaluation with imaging or biopsy.
3️⃣ Can fibroids cause infertility or pregnancy problems?
Yes. Fibroids that distort the uterine cavity may block the fallopian tubes or prevent embryo implantation.
They can also increase the risk of miscarriage, preterm labor, or breech position.
With proper treatment — such as myomectomy or uterine embolization — most women can achieve healthy pregnancies.
4️⃣ Can ovarian cysts cause infertility?
Some types of cysts, especially endometriomas (chocolate cysts) or cysts linked to polycystic ovary syndrome (PCOS), can interfere with ovulation and reduce fertility.
Treating the underlying hormonal imbalance or surgically removing the cyst often restores fertility.
5️⃣ Do fibroids or cysts go away on their own?
- ✅ Fibroids: Usually shrink after menopause or with hormonal therapy.
- ✅ Cysts: Functional cysts (from normal ovulation) often disappear naturally within 1–3 cycles.
Persistent, large, or painful cysts require medical attention.
6️⃣ What are the warning signs that I should see a doctor immediately?
Seek urgent medical help if you experience:
- ⚡ Sudden, severe lower abdominal pain
- 🩸 Heavy vaginal bleeding or large blood clots
- 🤢 Nausea, vomiting, or dizziness
- 🌡️ Fever with pelvic pain (possible infection)
- 🚨 Signs of cyst rupture or fibroid degeneration
7️⃣ Can fibroids or cysts come back after treatment?
Yes, recurrence can occur — especially if underlying hormonal imbalance persists.
Maintaining a healthy weight, balanced hormones, and regular gynecological check-ups helps reduce recurrence risk.
8️⃣ What is the difference between fibroids and ovarian cysts?
| Feature | Fibroids | Ovarian Cysts |
|---|---|---|
| Composition | Solid muscle tissue | Fluid-filled sac |
| Location | Uterus (muscle wall) | Ovary |
| Cancer Risk | Extremely low | Slightly higher (depends on type) |
| Common Symptoms | Heavy bleeding, pelvic pain | Abdominal pain, bloating |
| Fertility Impact | Uterine distortion | Ovulation problems |
9️⃣ How are fibroids and cysts diagnosed?
Diagnosis typically includes:
- 🩺 Pelvic examination
- 🖥️ Ultrasound (USG) for initial imaging
- 🧲 MRI for detailed evaluation
- 💉 Hormone or tumor marker tests
- 🔬 Hysteroscopy or laparoscopy, if needed for direct visualization or biopsy
🔟 How are fibroids and cysts treated without surgery?
- Fibroids: Medications (GnRH agonists, hormonal IUDs), or uterine fibroid embolization (UFE) — a non-surgical, uterus-preserving procedure.
- Cysts: Hormonal therapy or watchful waiting; surgery is only needed if cysts persist or twist (torsion).
11️⃣ Can diet or lifestyle changes help with fibroids and cysts?
Absolutely!
Adopting a healthy lifestyle can help prevent recurrence and manage symptoms:
- 🍎 Eat plenty of fruits, vegetables, and whole grains.
- 🥩 Limit red meat and processed foods.
- 🧘♀️ Exercise regularly and manage stress.
- ⚖️ Maintain a healthy weight.
- 💧 Stay hydrated and avoid alcohol or smoking.
12️⃣ Are fibroids or cysts painful?
Pain levels vary:
- Fibroids can cause pelvic pressure or menstrual cramps, especially during menstruation.
- Ovarian cysts can cause sharp, sudden pain if they twist or rupture.
Persistent or severe pain should always be evaluated by a healthcare provider.
13️⃣ What is uterine fibroid embolization (UFE)?
UFE is a minimally invasive procedure that blocks blood flow to fibroids, causing them to shrink over time.
Performed by an interventional radiologist, it allows women to avoid hysterectomy and preserve fertility.
Most patients go home the next day and recover within a week.
14️⃣ When should fibroids or cysts be surgically removed?
Surgery is considered if:
- Fibroids or cysts grow rapidly
- There is severe pain or heavy bleeding
- Fertility is affected
- There’s suspicion of malignancy
- Non-surgical treatments have failed
Procedures may include myomectomy, laparoscopy, or hysterectomy, depending on the case.
15️⃣ How can I prevent fibroids and cysts naturally?
While you can’t completely prevent them, you can lower risk through:
🌿 Balanced hormones, healthy diet, regular exercise, stress management, and annual gynecological exams.
16️⃣ Can fibroids or cysts return after menopause?
Usually no — after menopause, estrogen levels drop, and fibroids or cysts tend to shrink.
If they grow or reappear, further evaluation is needed to rule out other causes.
17️⃣ Are fibroids or cysts hereditary?
Yes, genetics play a significant role.
If your mother or sister had fibroids or cysts, your risk is higher.
Genetic predisposition is especially strong in uterine fibroids.
18️⃣ Can fibroids or cysts affect sexual life?
Yes.
- Fibroids can cause pain during intercourse (especially if near the cervix).
- Ovarian cysts can lead to pelvic tenderness or bloating.
Proper management and communication with your doctor help restore comfort and intimacy.
19️⃣ Can I get pregnant after fibroid or cyst treatment?
Most women can!
In fact, many women who struggled with infertility due to fibroids or cysts conceive successfully after proper treatment.
Your doctor will recommend the safest window for conception depending on your recovery.
20️⃣ What’s the best way to monitor my reproductive health?
👩⚕️ Regular gynecologic exams, annual pelvic ultrasounds, and maintaining awareness of your menstrual cycle are key to early detection and prevention.
Never ignore persistent pelvic pain or bleeding changes.
💡 Summary Tip:
Fibroids and cysts are common, treatable, and rarely dangerous when diagnosed early.
Stay proactive, listen to your body, and maintain regular check-ups. 🌸