🩺 Nutrition for Cancer Patients: The Cornerstone of a Healthy Life
One of the most important pillars in the fight against cancer is balanced and consistent nutrition.
Healthy eating not only strengthens the body but also supports treatment adherence, boosts immunity, and improves quality of life.
Because every individual’s needs are unique, nutrition plans should always be personalized.

🍽️ 1. The Importance of Balanced Nutrition
A healthy diet plays a key role both in cancer prevention and during treatment.
Providing the body with enough energy, protein, vitamins, and minerals helps the immune system stay strong and resilient.
Main goals of a healthy diet:
- Maintain an ideal body weight
- Ensure dietary variety
- Consume sufficient fluids
- Avoid processed foods
🥦 2. The Five Essential Food Groups
Include these five food groups in your meals every day:
- Protein sources: Meat, chicken, fish, eggs, legumes
- Fruits and vegetables: A colorful variety from all groups
- Whole grains: Whole wheat bread, bulgur, oats
- Dairy products: Yogurt, kefir, ayran, cheese
- Fluids: Water, ayran, herbal tea, mineral water
🔹 Remember: There are no miracle diets. The key is a natural, balanced, and hygienic eating routine.
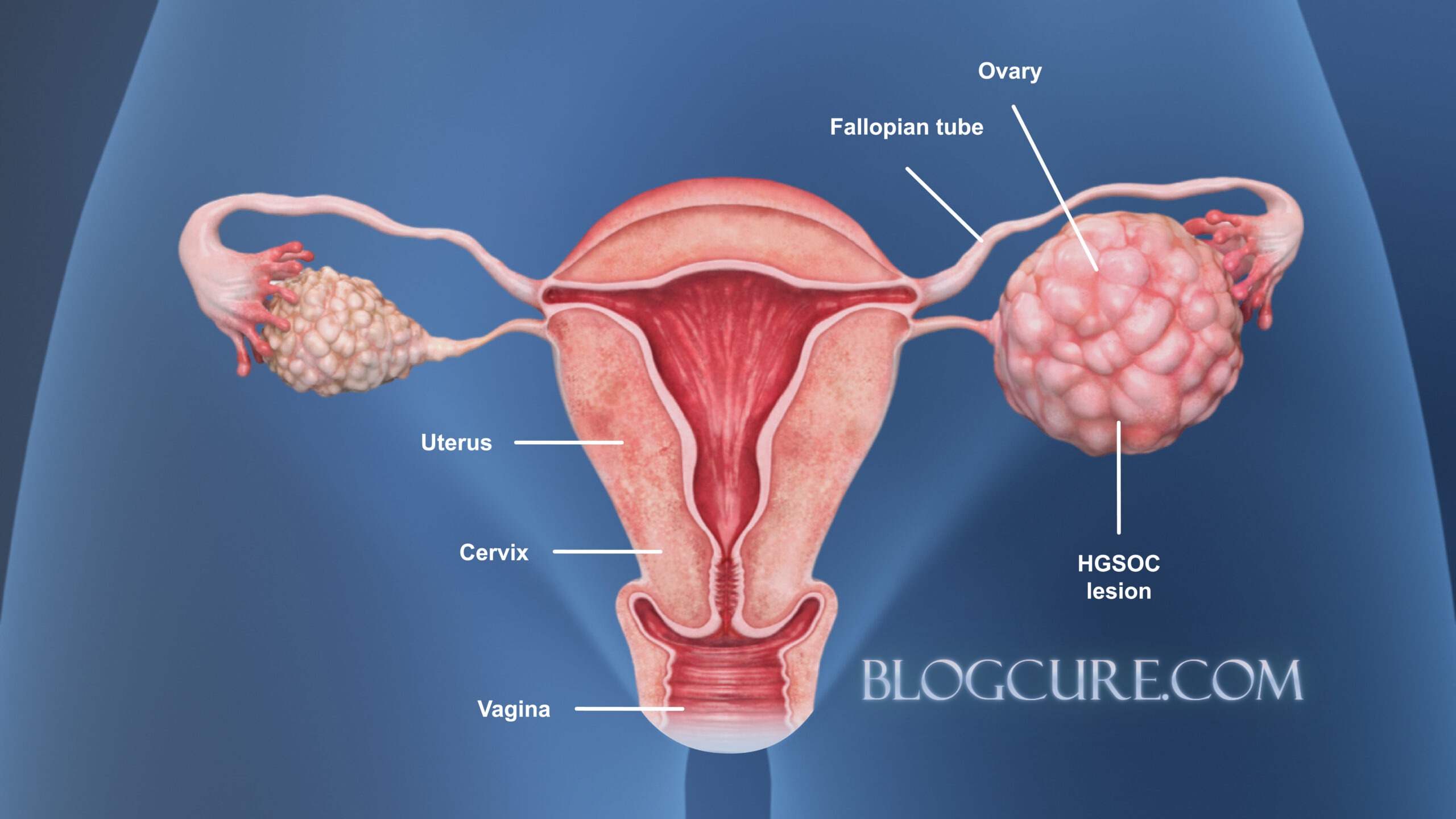
🧬 3. Personalized Nutrition Planning
A cancer patient’s energy and nutrient requirements depend on several factors:
- Type of treatment
- Stage of the disease
- Body weight
- Age and physical activity level
Therefore, nutrition should always be planned under the supervision of a doctor and dietitian.
Ready-made or trendy diets have no proven scientific benefit in cancer treatment.
💧 4. Nutrition During Chemotherapy
During chemotherapy, nausea, vomiting, taste changes, mouth sores, loss of appetite, and fatigue are common.
The main goal is to restore lost energy and maintain fluid balance.
🔹 Fluid Intake
- Drink 2–2.5 liters of fluid daily (unless your doctor advises otherwise).
- Fluids include not only water but also ayran, herbal tea, mineral water, and fresh juices.
- Avoid grapefruit and pomegranate juice, as they may interact with some chemotherapy drugs — always consult your doctor first.
🔹 Mouth Sores and Irritation
- Avoid acidic, spicy, pickled, or very hot foods.
- Eat meals at room temperature or slightly warm.
- Choose gentle cooking methods like steaming, boiling, or baking.
🔹 Variety in Fruits and Vegetables
- Consume at least five servings of different-colored fruits and vegetables daily.
- Color diversity increases the intake of protective phytochemicals.
- Prefer dark leafy greens, citrus fruits, and root vegetables like carrots, beets, and squash.
🔹 Fat Use
- Replace saturated fats (butter, lard) with healthy vegetable oils like olive oil.
- Avoid processed meats such as sausages, salami, and cured meats.

🤢 5. Coping with Nausea and Vomiting
Chemotherapy-induced nausea and vomiting can greatly reduce food intake.
To make eating easier during this phase:
- Eat small, frequent meals (6–8 times a day).
- Keep rooms well ventilated and avoid strong food odors.
- Choose soft, light, and odorless foods.
- Mint or lemon-flavored candies can help ease nausea.
- Stay hydrated with ayran, fruit juice, or mineral water.
- If vomiting is severe, consult your doctor immediately — fluid and electrolyte loss can be dangerous.
🥣 6. Managing Loss of Appetite
Loss of appetite is common during both chemotherapy and radiotherapy.
If it persists, it may lead to weight loss and muscle wasting.
The goal is to support the body with small but nutrient-dense meals.
Keep healthy snacks within reach:
- Yogurt, milk-based desserts, nuts, small sandwiches, boiled eggs, cheese sticks, or stewed fruits.
Tips:
- Choose high-protein, high-energy foods.
- If main meals are unappealing, eat breakfast-style foods instead.
- Make meals visually appealing — colorful plates, a pleasant table setup, or your favorite music can help.
- Light exercise or short walks (if approved by your doctor) may stimulate appetite.
- When necessary, your dietitian may recommend enteral nutrition products (medical nutrition supplements).
👃 7. Changes in Taste and Smell
During chemotherapy, many patients experience metallic or bitter tastes and altered smell perception.
To reduce these effects:
- Rinse your mouth frequently and maintain good oral hygiene.
- Try sugar-free mint or lemon-flavored candies.
- Use plastic utensils instead of metal ones.
- Add natural flavorings like basil, rosemary, garlic, or yogurt to meals.
- If you have difficulty eating red meat, substitute with fish, chicken, eggs, dairy, or legumes.
- Blend fresh fruits with yogurt or milk to make smoothies.
- Choose cold or room-temperature foods if cooking smells bother you.
🧡 8. Conclusion: Healthy Nutrition, Strong Immunity
In cancer treatment, nutrition supports not only physical strength but also mental well-being.
Each patient’s body is different — there is no universal “miracle diet.”
Remember:
- The best approach is a balanced, hygienic, and personalized diet.
- Never make major dietary changes without consulting your doctor or dietitian.
- With small, consistent steps, you can build a nutrition routine that truly supports your recovery.
FAQ – Nutrition for Oncology Patients
1. What should I eat during chemotherapy?
During chemotherapy, focus on small, frequent meals that are nutrient-dense. Include proteins, whole grains, fruits, vegetables, and fluids. Avoid very spicy, acidic, or greasy foods if they worsen nausea or mouth sores.
2. How can I manage loss of appetite?
- Eat smaller portions more frequently (6–8 times/day).
- Keep high-protein snacks handy: yogurt, boiled eggs, cheese, nuts, smoothies.
- Make meals visually appealing and eat in a calm, well-ventilated environment.
- Light exercise, such as short walks, may help stimulate appetite (if approved by your doctor).
3. What fluids should I drink?
Aim for 2–2.5 liters daily, including water, herbal tea, ayran, mineral water, and diluted juices. Avoid grapefruit or pomegranate juice without checking with your doctor, as some may interact with chemotherapy drugs.
4. How can I cope with nausea and vomiting?
- Eat soft, bland, and odorless foods.
- Avoid strong cooking smells.
- Try mint or lemon-flavored candies to reduce nausea.
- Stay hydrated with fluids.
- If vomiting is severe, contact your doctor immediately.
5. What if food tastes or smells different?
- Rinse your mouth regularly and maintain good oral hygiene.
- Use sugar-free mint or lemon candies.
- Eat room-temperature or cold foods to reduce cooking odors.
- Add flavor with herbs like basil or rosemary, or condiments like yogurt or sauces.
6. Are there any foods I should completely avoid?
- Highly processed meats such as sausages, salami, and cured meats
- Very greasy, fried, or extremely spicy foods
- Very hot or acidic foods if they irritate mouth sores
7. Can I still enjoy my favorite foods?
Yes, but modify textures or temperatures as needed. For example, blend fruits into smoothies, eat cooked vegetables instead of raw, or have cold dishes if hot food smells trigger nausea.
8. Do I need special supplements or medical nutrition products?
Sometimes enteral nutrition products or protein-rich supplements may be recommended by your dietitian to meet calorie and protein needs. Always consult your doctor or dietitian before using them.
9. How important is a personalized nutrition plan?
Very important. Each patient’s needs vary depending on treatment type, disease stage, weight, age, and activity level. A personalized plan ensures adequate nutrition, supports immunity, and reduces treatment side effects.
10. Can proper nutrition improve treatment outcomes?
Yes. Balanced nutrition helps maintain energy levels, prevents excessive weight loss, strengthens immunity, and can improve overall quality of life during treatment.