Radiotherapy: A Comprehensive Guide 🩺💡
What is Radiotherapy?
Radiotherapy is a medical treatment that uses ionizing radiation to target and destroy cancer cells. It is one of the primary cancer treatment methods, alongside surgery and chemotherapy. Radiotherapy can be applied alone or in combination with other treatments, either before or after surgery, before, after, or simultaneously with chemotherapy.
Radioactive rays work by destroying cancer cells in the treated area. Normal cells in the same region may also be affected, but they generally have the ability to repair themselves, making radiation-related damage mostly temporary.
To minimize potential side effects, the total radiation dose is usually divided into multiple sessions. Typically, treatment occurs five days a week, with one session per day, allowing normal cells to recover over the weekend.
Different radiotherapy devices and techniques are chosen based on the patient’s overall health, cancer type, and disease stage. Treatment can be delivered either:
- Externally (from outside the body)
- Internally (placing radioactive substances inside body cavities or tissues)
The treatment plan is highly individualized, considering factors such as the patient’s age, health status, cancer type, stage, and tumor location. Decisions are made collaboratively by specialists from multiple medical disciplines, ensuring each patient receives a personalized plan—even if two patients have the same type of cancer.
⚠️ Important: Radiotherapy is never contagious.
Safety and Social Considerations
Radiotherapy does not make you radioactive. You do not emit radiation, so you can safely interact with family, friends, and children during and after treatment. There is no need to separate personal belongings at home.
Goals of Radiotherapy 🎯
Radiotherapy can be categorized into two main goals:
1. Curative (Curative Intent)
This type aims to completely eradicate the disease based on current medical knowledge. It can be used alone or combined with surgery and/or chemotherapy.
2. Palliative (Symptom Relief)
The goal here is not to cure, but to relieve symptoms and improve quality of life. For example:
- Radiation to a painful bone can reduce pain
- Radiation to bleeding tumors can control bleeding
Types of Radiotherapy Applications
Radiotherapy is mainly classified by how it is applied:
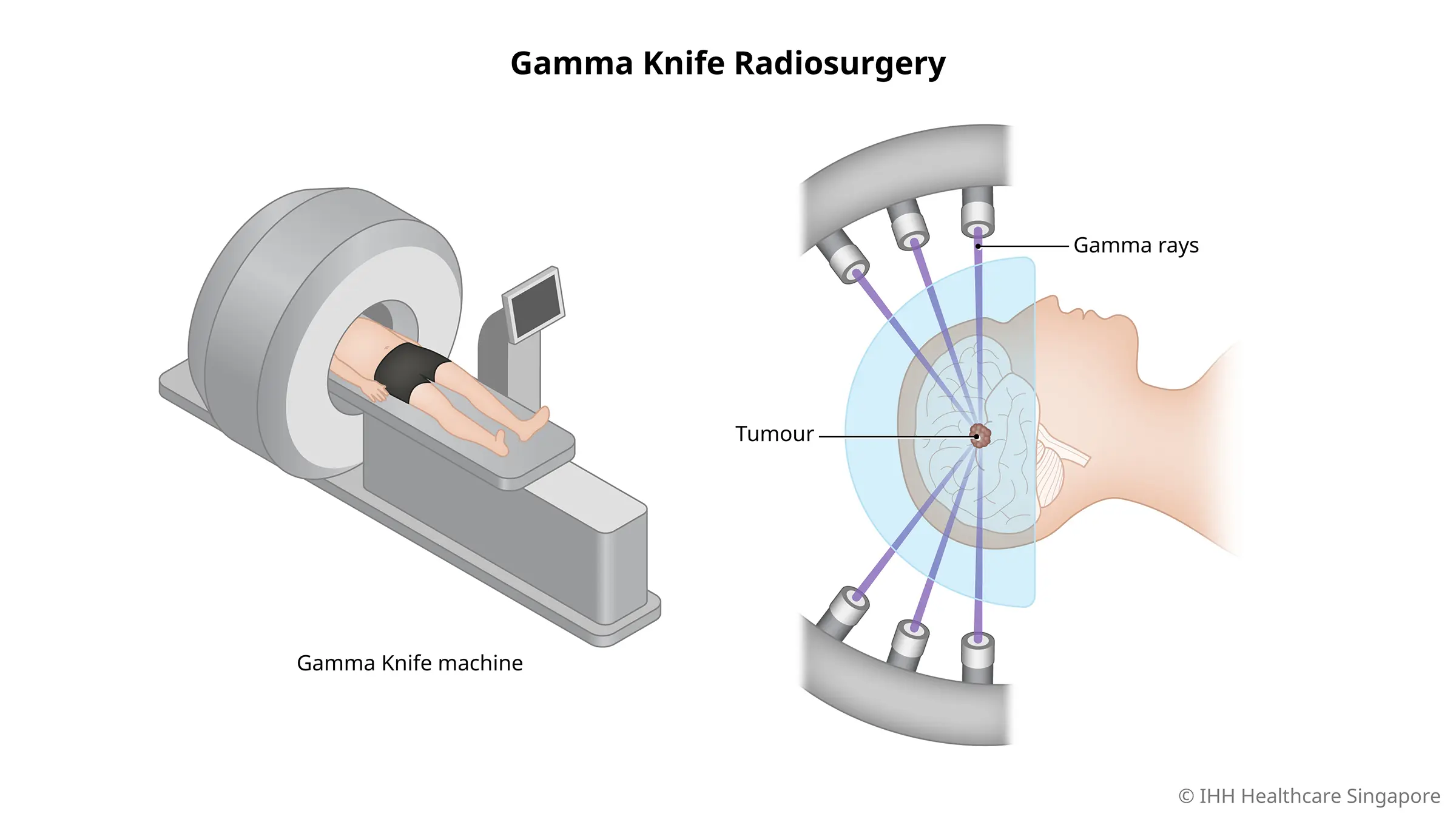
External Radiotherapy (External Beam Radiation)
- Patients usually do not stay in the hospital overnight; treatments are outpatient.
- High-energy X-rays are produced by a machine and directed at the tumor from outside the body.
Internal Radiotherapy (Brachytherapy)
- Radiation is delivered from inside the body using various techniques.
- The main goal is to deliver high doses to the tumor while protecting surrounding healthy tissue.
Brachytherapy (Internal Radiation) 💉
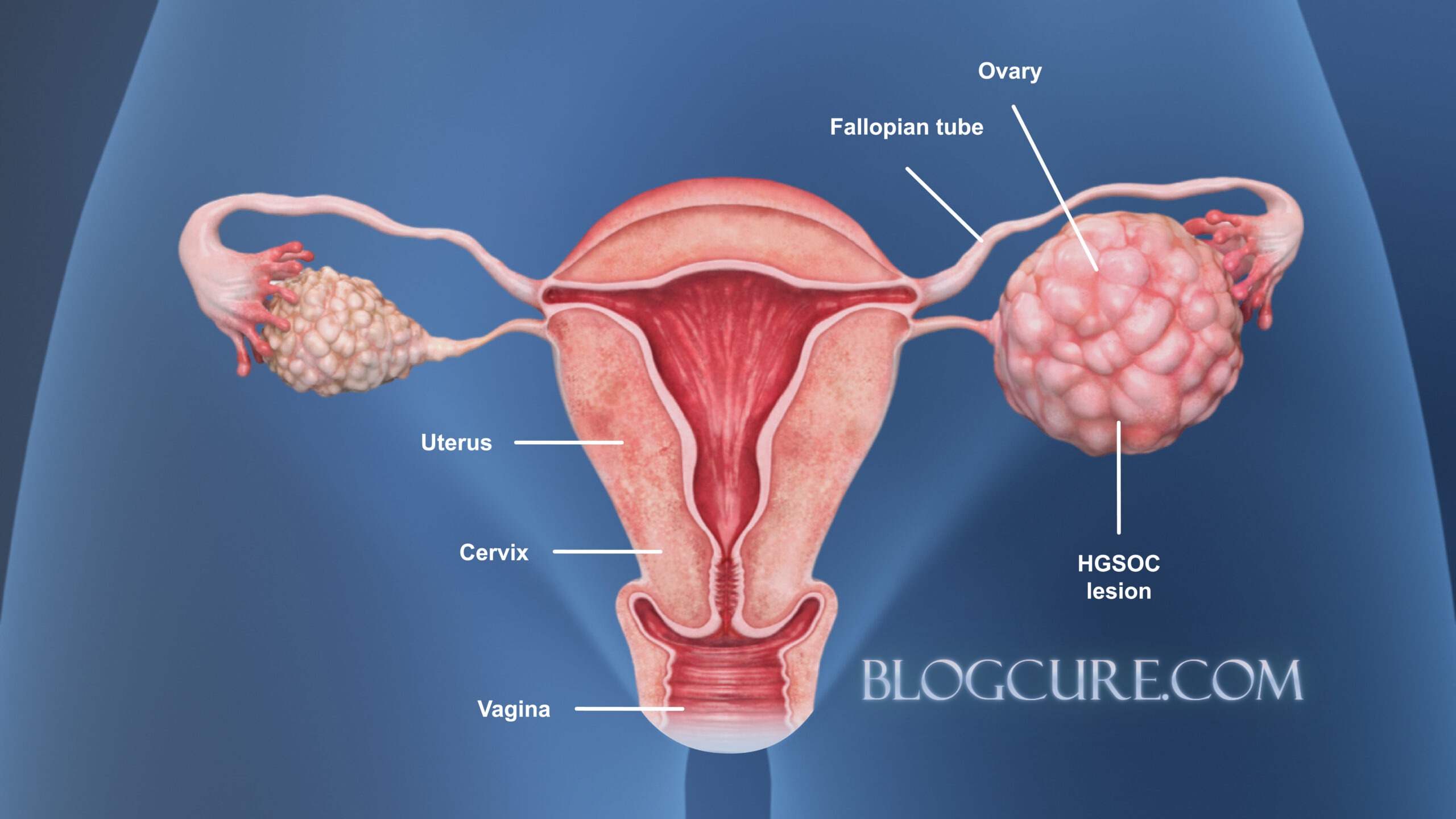
Intracavitary Therapy
- Radioactive sources are placed inside body cavities using special applicators.
- Most commonly used in female reproductive cancers, like uterine or cervical cancer.
- Often follows external radiotherapy to increase the dose to the target area.
- Our clinic uses 3D High Dose Rate (HDR) Brachytherapy with Iridium-192.
Interstitial Therapy
- Radioactive sources are inserted directly into the tissue surrounding the tumor.
- Frequently used for cancers in the breast, lips, or oral cavity.
- Ideal for local recurrences after prior external radiotherapy, as it minimizes damage to surrounding healthy tissue.
- Commonly uses Iridium-192 or Cobalt-60, delivered via thin needles, wires, or tubes under local or general anesthesia.
External Radiotherapy: Planning and Procedure 📋
External radiotherapy is delivered from outside the body, following a treatment plan determined by the radiation oncologist based on:
- Patient condition
- Cancer type and stage
- Treatment objectives
Frequency of Treatment
- Total radiation dose is divided into smaller daily doses
- Typically administered five days a week
- Treatment duration can range from 1 day to 8 weeks
- Patients are fully briefed by their physician and must sign informed consent
Simulation and Preparation for Radiotherapy
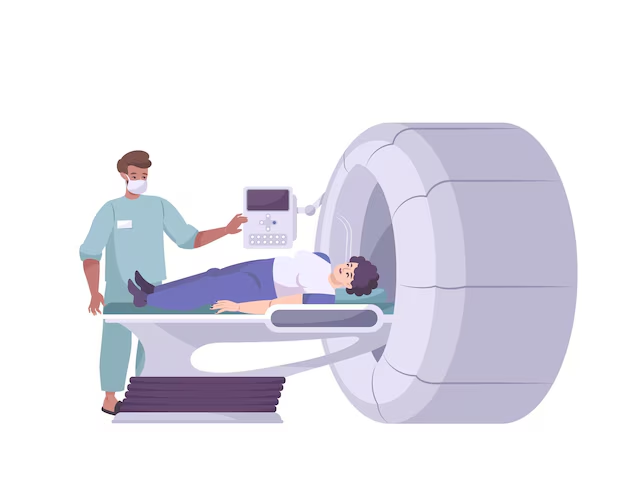
Before treatment, patients undergo CT simulation to:
- Determine the best treatment position
- Acquire imaging for precise planning
Immobilization Accessories
- Devices ensure reproducible and comfortable positions during treatment. Examples:
- Head and neck: custom thermoplastic masks, vacuum cushions
- Other regions: lung boards, breast boards, abdominal flattening cushions, leg supports
- Color lasers or tattoos may be used to mark positioning points.
Imaging for Treatment Planning
- CT scans identify the treatment area and organs at risk
- Sometimes additional measures are used to enhance imaging, such as oral or IV contrast
During the First Treatment Session
- Treatments are pain-free and last a few seconds to several minutes
- Technicians ensure correct positioning using previously marked points
- Patients remain alone in the treatment room, but a microphone and camera system allow continuous monitoring
Treatment Delivery and Guidance (IGRT)
- Image-Guided Radiotherapy (IGRT) ensures precise positioning and targeting
- Machines may rotate 360 degrees around the patient for multi-angle treatment
- Technicians adjust or pause treatment if the patient moves
- Daily appointment adherence is crucial for optimal results
Radiotherapy Team 👩⚕️👨⚕️
- Radiation Oncologist: Leads the treatment plan
- Medical Physicist: Calculates doses and ensures device safety
- Radiotherapy Technician: Administers the treatment
- Oncology Nurse: Provides patient care and information on side effects
- Other Support Staff: Psychologists, dietitians, physiotherapists, social workers
Your role is crucial:
- Arrive on time for sessions
- Ask questions and share concerns
- Report side effects promptly
- Follow advice from the care team
Emotional Well-Being During Radiotherapy 💚
It is normal to experience:
- Anxiety
- Stress
- Fear
- Frustration
- Helplessness
- Loneliness
Cancer treatment is emotionally challenging, and these feelings may contribute to fatigue. Support is available through the care team.
Managing Emotions and Side Effects During Radiotherapy 🌿💛
Coping with Emotions During Radiotherapy 🧘♀️
It’s completely normal to experience a wide range of emotions during your radiation treatment. You may feel:
- Anxious
- Depressed or overwhelmed
- Afraid or frustrated
- Hopeless or lonely
To help manage these emotions, try the following strategies:
Relaxation and Meditation
- Listen to calming music while breathing slowly and mindfully
- Imagine yourself in a favorite, peaceful place
- These techniques can help you feel calmer and less stressed
Talk About Your Feelings
- Speak with your doctor, nurse, or radiation oncologist
- If needed, meet with a clinical psychologist specializing in oncology
Exercise
- Light physical activity, such as cycling, yoga, swimming, aerobics, or walking, can boost well-being
- Discuss appropriate exercises with your doctor or nurse
Social Support
- Share your feelings with someone you trust (friend, family member, religious advisor, nurse, social worker, psychologist)
- Join a cancer support group to meet people experiencing similar challenges
- Hospitals may offer Occupational Therapy Units or Cancer Patient Schools to provide guidance and social support
Radiotherapy Side Effects and Coping Strategies ⚕️
Side effects of radiotherapy can vary widely from person to person. They may be mild, pronounced, or absent. Side effects are classified as:
- Early side effects (appear during or shortly after treatment)
- Late side effects (appear months or years later)
Always report any side effects to your nurse or doctor. The following guidance is for informational purposes only and does not replace medical advice.

Common Side Effects by Treatment Area
- Diarrhea 💧
- Fatigue 😴
- Hair and beard loss 💇♀️
- Oral changes 👄
- Nausea and vomiting 🤢
- Changes in sexual health and fertility ❤️
- Urinary and bladder changes 🚽
- Skin reactions 🌿
- Throat changes 🗣️
Diarrhea 💧
What it is: Frequent, loose, or watery bowel movements caused by radiation in the abdominal or pelvic area.
Why it happens: Radiation may damage healthy cells in the intestines.
Coping strategies:
- Drink 8–12 glasses of fluids daily (water, juice, iced tea, ayran, soda)
- Eat small, frequent meals
- Choose foods low in fiber, fat, and lactose
- For severe diarrhea: bananas, rice, apples, peaches, boiled potatoes, toast, and salty ayran
- Clean gently after bowel movements; report rectal irritation to your doctor
Avoid:
- Milk, spicy foods, hot sauces, curries
- Gas-producing foods (beans, chickpeas, cabbage, broccoli, soy, nuts)
- Raw vegetables, whole grains, high-fiber foods
- Fried or fast food
Fatigue 😴
What it is: Common and varies by individual; may begin gradually during treatment.
Causes:
- Anemia
- Stress or anxiety
- Depression
- Infection
- Reduced activity
- Medication side effects
- Effort spent traveling to treatment
Duration: Fatigue can last 6 weeks to 12 months after starting radiotherapy.
Coping strategies:
- Aim for 8 hours of sleep per night
- Stay active: yoga, walking, or light cycling
- Use short naps (under 1 hour) during the day
- Prioritize activities that are most important to you
- Discuss exercise plans with your care team
- Plan daily schedules and adjust work hours if needed
- Seek support from family, friends, or support groups
- Consult your doctor if fatigue is related to anemia, depression, or sleep issues
Hair Loss 💇♀️
What it is: Partial or complete hair loss in the treatment area (scalp, pelvic area, or other regions).
Why it happens: Radiation can damage hair follicles in the treated region.
Duration and recovery:
- Hair loss may begin 2–3 weeks after the first session
- Hair may regrow 3–6 months post-treatment
- Regrown hair may be different in color, texture, or thickness
Coping tips:
- Use gentle shampoos and soft towels
- Avoid hair dryers, curling irons, hair products, or chemical treatments
- Protect your scalp with hats or scarves, especially from extreme temperatures or sunlight
- Consider trimming hair before treatment begins
- Purchasing a wig before hair loss ensures a closer match to your natural hair
Oral Changes
Radiation in the head and neck region may cause:
- Mouth sores or ulcers
- Dry mouth
- Tooth decay
- Altered taste (metallic or loss of taste)
- Gum, tooth, or tongue infections
- Jaw stiffness
- Thick saliva
Why it happens: Radiation can affect salivary glands, soft tissues, and mucosa while targeting cancer cells.
Coping strategies:
- Maintain excellent oral hygiene with soft brushes and gentle rinses
- Use fluoride toothpaste or gels as recommended
- Avoid alcohol-based mouthwashes
- Drink water frequently and chew sugar-free gum
- Eat soft, moist foods (mashed potatoes, scrambled eggs, soft grains)
- Avoid acidic, spicy, hot, or crunchy foods
- Consult your care team regarding medications or mouth care solutions
- Perform jaw exercises 3 times daily
Important: Avoid tobacco and alcohol, as they reduce treatment effectiveness and increase side effect severity
Nausea and Vomiting 🤢
What it is: Radiation in the abdomen, pelvis, or head region can trigger nausea or vomiting.
Why it happens: Depends on treatment site, radiation dose, and concurrent chemotherapy
Duration: Symptoms may occur 30 minutes to hours after treatment and usually improve on non-treatment days.
Coping strategies:
- Eat small, frequent meals (5–6 meals instead of 3)
- Eat mild, easy-to-digest foods
- Allow foods and drinks to cool to moderate temperature before consuming
- Relax before sessions with music, reading, or calming activities
- Consult your doctor for anti-nausea medications or special diets
💊 Sexual Health & Fertility Changes During Radiation Therapy
Radiation therapy in the pelvic region can impact sexual function and fertility. Understanding these changes and ways to cope can help patients maintain quality of life during and after treatment.
⚠️ Why Sexual Health Can Be Affected
Pelvic radiation may affect sexual organs and hormonal balance, leading to:
- Loss of sexual function
- Changes in libido
- Infertility
These effects differ between men and women.
👩 Women: Common Effects
Radiation targeting the vagina, uterus, and ovaries may cause:
- Pain or discomfort during sexual activity
- Vaginal dryness, itching, burning, or atrophy (thinning of vaginal walls)
- Vaginal stenosis (narrowing and loss of elasticity)
- Menopause-like symptoms (hot flashes, vaginal dryness)
Other contributing factors include fatigue, anxiety, depression, and scar tissue from prior treatments.
Coping Strategies:
- Fertility: Discuss egg preservation or fertility options with your doctor before starting treatment.
- Sexual Health: Seek guidance on potential sexual side effects.
- Contraception: Radiation can harm a fetus at any stage. Discuss birth control and pregnancy plans with your healthcare provider.
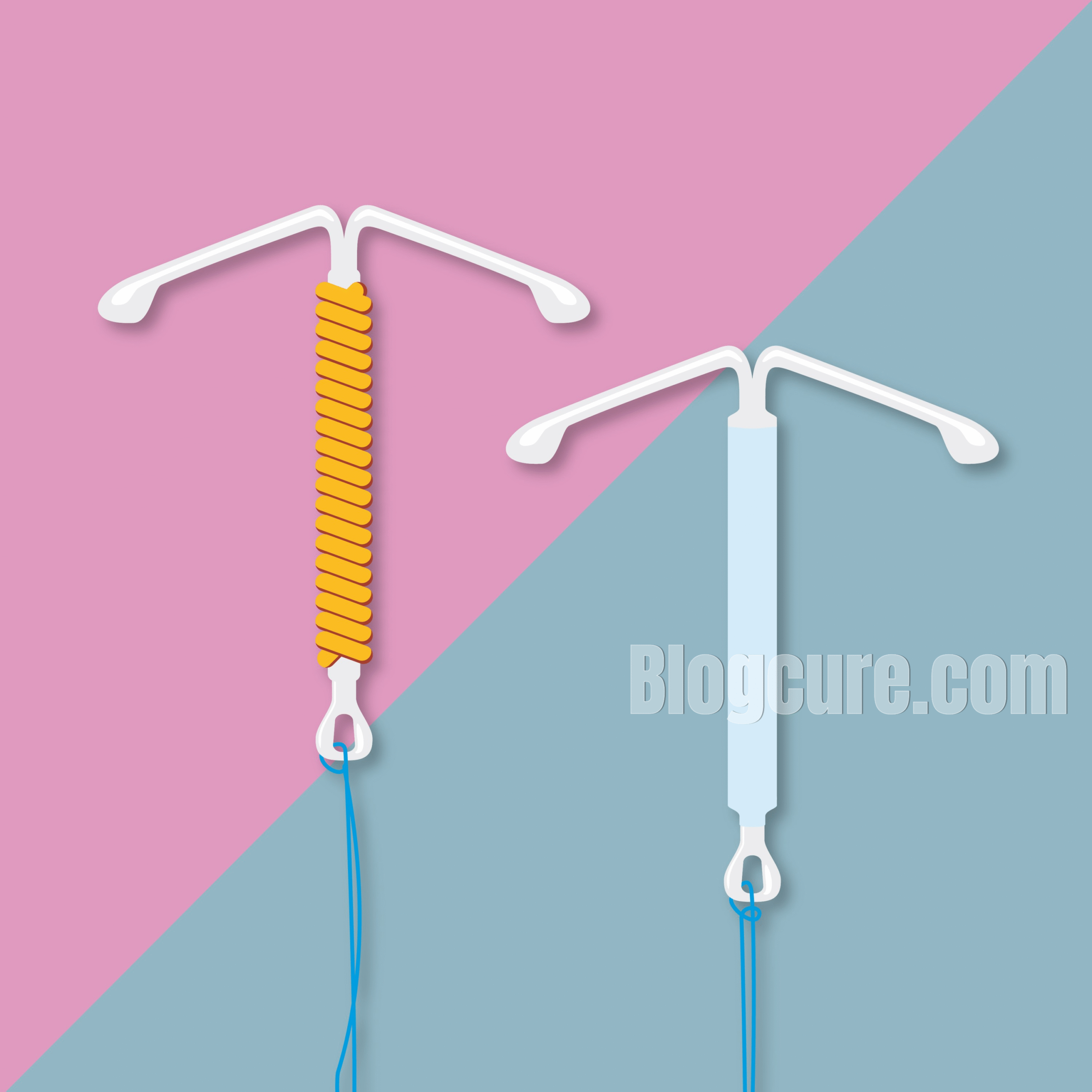
- Vaginal Dilators & Moisturizers: Dilators help prevent narrowing, and lubricants or water-based gels can reduce dryness.
👨 Men: Common Effects
Radiation may impact erectile function and sperm quality, leading to:
- Erectile dysfunction
- Reduced sperm count or infertility
Coping Strategies:
- Fertility: Consider sperm banking before treatment.
- Erectile Dysfunction: Ask your doctor about medications or other treatment options.
- Sexual Activity: Discuss concerns about sexual activity during therapy.
🤝 Shared Advice for Men & Women
- Open Communication: Share sexual health concerns with your partner.
- Fertility Preservation: Plan ahead if you wish to have children post-treatment.
🚽 Urinary & Bladder Changes
Pelvic radiation can also affect the urinary system, causing:
- Burning or pain while urinating
- Incomplete bladder emptying
- Frequent urination, nighttime urination
- Urinary infections (cystitis)
- Urinary incontinence
- Blood in urine
- Bladder cramps
Causes: Healthy cells in the bladder and urinary tract may be damaged, leading to inflammation, ulceration, or infection.
Recovery Timeline: Symptoms often appear 3–5 weeks into therapy and improve within 2–8 weeks after completion.
Coping Strategies:
- Drink 6–8 glasses of water daily (urine should be pale yellow).
- Avoid alcohol, coffee, spicy foods, and tobacco.
- Perform bladder control exercises if recommended.
- Take prescribed medications for infection, pain, or spasms.
🧴 Skin Changes
Radiation can affect the skin in various ways:
- Redness or darker patches
- Itching
- Dryness or peeling
- Moisture-related reactions (under breasts, behind ears, or in skin folds)
- Swelling (edema)
Causes: Radiation damages skin cells, preventing regeneration during treatment.
Recovery Timeline: Skin reactions may start within weeks and often improve gradually after therapy. However, permanent changes like darkening or sensitivity to sunlight can persist.
Coping Strategies:
- Use doctor-recommended creams or lotions.
- Avoid extreme temperatures on the skin (hot/cold packs).
- Take lukewarm showers; avoid harsh soaps.
- Wear soft, breathable clothing; avoid tight garments.
- Protect skin from the sun using SPF 30+ and long clothing.
- Report severe skin changes to your healthcare provider.
🗣️ Throat & Esophagus Changes
Radiation to the neck or chest can lead to:
- Pain or inflammation (esophagitis)
- Difficulty swallowing
- Sensation of a burning lump
Causes: Healthy cells in the throat may be damaged. Smoking or alcohol can worsen symptoms.
Recovery Timeline: Symptoms usually start 2–3 weeks into treatment and improve 4–6 weeks after completion.
Coping Strategies:
- Eat soft, moist foods like mashed potatoes, scrambled eggs, or porridge.
- Take small, frequent meals.
- Avoid very hot, spicy, acidic, or crunchy foods.
- Use liquids to soften food.
- Prioritize high-protein, high-calorie foods to maintain weight.
🏥 Brachytherapy Procedures
Brachytherapy involves placing radioactive sources inside or near the tumor. Often used in gynecologic cancers (cervical or uterine). It can be performed outpatient, without hospital admission.
For Patients With Surgery:
- Usually applied 2–5 times, weekly.
- No external radiation on brachytherapy days.
- Pre-procedure: light meal allowed; medications for hypertension or diabetes may be taken.
- Procedure: applicator is inserted into the vagina; bladder may be catheterized. Monitored via video camera.
- Post-procedure: applicator and catheter removed; drink plenty of fluids. No radiation remains in your body.
For Patients Without Surgery:
- Typically 4 sessions, weekly or biweekly.
- Procedure performed under anesthesia; monitored by nurse and physicist.
Vaginal Dilator Therapy:
- Helps prevent narrowing.
- Begin 2 weeks post-treatment: use 3 times per week for 10 minutes.
- Lubricants or baby oil can reduce discomfort.
- Gradually progress through dilator sizes; mild bleeding may occur and is normal.
✅ Key Takeaways:
- Radiation therapy can affect sexual health, fertility, urinary system, skin, and throat.
- Most side effects improve after treatment, but some may persist.
- Open communication with your healthcare provider, partner, and support network is crucial.
- Preventive measures like fertility preservation, skin care, bladder exercises, and dilator therapy can greatly improve quality of life.
Table 1: Sexual Health & Fertility Changes During Radiation Therapy
| Patient Group | Common Side Effects | Possible Duration | Coping Strategies / Interventions |
|---|---|---|---|
| Women | Pain during intercourse, vaginal dryness, itching, burning, vaginal stenosis, menopause symptoms | Weeks to months after treatment; some changes may persist | Vaginal dilators, lubricants, fertility preservation (egg freezing), counseling |
| Men | Erectile dysfunction, reduced sperm count, infertility | Weeks to months after treatment; usually improves | Sperm banking, medications for ED, counseling, open communication with partner |
Table 2: Urinary & Bladder Changes
| Symptom | Cause | Typical Onset | Management |
|---|---|---|---|
| Burning / pain during urination | Damage to bladder and urethra | 3–5 weeks into therapy | Hydration (6–8 glasses/day), avoid caffeine/alcohol, medications if prescribed |
| Frequent urination / nocturia | Irritation of bladder lining | 3–5 weeks into therapy | Bladder training exercises, fluid management |
| Urinary incontinence | Weakening of pelvic floor muscles | During or post-treatment | Pelvic floor exercises, consult urologist |
| Hematuria (blood in urine) | Tissue inflammation, ulceration | During treatment | Report to doctor immediately |
Table 3: Skin Changes Due to Radiation Therapy
| Type of Change | Description | Timing | Management / Prevention |
|---|---|---|---|
| Redness / hyperpigmentation | Skin looks sunburned or darker | Starts within weeks of therapy | Use doctor-recommended creams, avoid harsh soaps, gentle washing |
| Itching | Persistent pruritus in treated area | During therapy | Moisturizers, avoid scratching |
| Dryness / peeling | Skin loses moisture, may peel | During therapy | Regular application of prescribed emollients, stay hydrated |
| Moisture-related reactions | Rash or ulceration in skin folds | During therapy | Keep area dry and ventilated |
| Swelling (edema) | Puffy appearance in treated area | During therapy | Compression garments if recommended, monitor changes |
Table 4: Throat & Esophageal Changes
| Symptom | Cause | Onset | Management |
|---|---|---|---|
| Sore throat / burning sensation | Radiation-induced inflammation (esophagitis) | 2–3 weeks into therapy | Soft, moist foods; avoid spicy/acidic foods; hydration |
| Difficulty swallowing | Damage to healthy throat tissue | 2–3 weeks into therapy | Small, frequent meals; food thickened with sauces, yogurt, or liquids |
| Sensation of lump / tightness | Swelling or irritation | 2–3 weeks into therapy | Cold/room-temperature foods; avoid hot drinks |
Table 5: Brachytherapy Guidelines & Vaginal Dilator Use
| Patient Type | Sessions / Frequency | Key Steps Before Procedure | During Procedure | After Procedure / Home Care |
|---|---|---|---|---|
| Post-surgery (cylinder applicator) | 2–5 weekly sessions | Light meal, medication review, empty bladder, optional laxative | Applicator insertion, bladder catheterization, monitored via video | Applicator & catheter removal, drink plenty of fluids (2+ L), report urinary or GI issues |
| No surgery (INOP) | 4 sessions, weekly or biweekly | Fasting overnight, medication review, empty bladder, lavman | Anesthesia, applicator insertion, monitored | Same as above; may experience temporary dizziness, nausea, or drowsiness |
| Vaginal dilator therapy | 2 weeks post-treatment, 3x/week, 10 minutes | Use lubricant, start with smallest dilator | Gently insert, do not force; mild bleeding is normal | Progress through sizes weekly, wash dilator before & after, continue until first gynecological check-up |
Radiation Oncology FAQ – Frequently Asked Questions
💖 Sexual Health & Fertility
❓ Can radiation therapy affect sexual function or fertility?
Yes. Radiation to the pelvic area can cause changes in sexual desire, erectile dysfunction in men, vaginal dryness or stenosis in women, and potential infertility. Effects vary depending on gender and treatment site.
❓ What sexual problems can women experience after pelvic radiation?
- Pain during intercourse
- Vaginal dryness, burning, or itching
- Vaginal stenosis (narrowing and loss of elasticity)
- Menopause symptoms (hot flashes, vaginal atrophy)
❓ How can women cope with these changes?
- Use vaginal dilators as recommended
- Lubricants or water/oil-based gels
- Open communication with partners
- Fertility preservation (egg freezing) before therapy
❓ What sexual problems can men experience?
- Erectile dysfunction
- Reduced sperm count or infertility
❓ How can men manage fertility and sexual side effects?
- Sperm banking before treatment
- Medications or devices for erectile dysfunction
- Open communication with partners
❓ Do these side effects go away?
Many sexual side effects improve gradually after treatment ends, but some changes may persist. Regular follow-ups with your doctor help manage long-term effects.
🩺 Urinary & Bladder Issues
❓ What urinary problems can radiation therapy cause?
- Burning or pain while urinating
- Incomplete bladder emptying
- Frequent urination or nocturia
- Urinary tract infections (cystitis)
- Urinary incontinence
- Blood in urine
- Bladder cramps
❓ Why do these occur?
Radiation can damage healthy cells in the bladder and urinary tract, causing inflammation, ulceration, or infection.
❓ How long do urinary side effects last?
Symptoms usually start 3–5 weeks into therapy and improve within 2–8 weeks after treatment.
❓ How can I manage urinary side effects?
- Drink 6–8 glasses of water daily
- Avoid alcohol, caffeine, and spicy foods
- Perform pelvic floor exercises if recommended
- Use prescribed medications for infection, pain, or spasms
🧴 Skin Changes
❓ What skin changes can radiation therapy cause?
- Redness or mild-to-severe erythema
- Itching
- Dryness, peeling, or flaking
- Moist reactions in skin folds (under breasts, ears, perineum)
- Swelling or edema
❓ Why do skin changes occur?
Radiation damages skin cells, preventing normal regeneration during therapy.
❓ How long do skin changes last?
They often appear a few weeks after therapy begins and improve gradually after treatment. Some discoloration or thickness may persist.
❓ How to take care of my skin during radiation therapy?
- Use doctor-recommended creams and moisturizers
- Avoid hot/cold packs and harsh soaps
- Wear soft cotton clothing and avoid tight garments
- Protect skin from sunlight with SPF 30+ or protective clothing
- Keep treated areas clean and dry, and follow medical instructions carefully
🫁 Throat & Esophageal Issues
❓ Can radiation affect my throat or swallowing?
Yes. Radiation to the neck or chest can cause pain, a burning sensation, lump feeling, and difficulty swallowing (esophagitis).
❓ How can I manage throat problems?
- Eat soft, moist foods
- Consume small, frequent meals (3 main + 3 snacks)
- Moisten food with sauces, broths, or yogurt
- Avoid spicy, acidic, or very hot foods
- Drink cool or room-temperature beverages
❓ How long do throat symptoms last?
Symptoms usually improve 4–6 weeks after treatment ends.
❓ How can I maintain nutrition during therapy?
- Choose high-calorie, high-protein foods
- Blend foods if necessary to ease swallowing
- Consult a dietitian if you lose weight or struggle to eat
☢️ Brachytherapy
❓ What is brachytherapy?
Brachytherapy is a treatment in which radioactive sources are placed inside or near the tumor. It is often used for gynecological cancers (cervix, uterus) either alone or with external beam radiation.
❓ Do I need to stay in the hospital?
Usually no. Most patients receive brachytherapy as an outpatient procedure.
❓ Can I have sex during brachytherapy?
Sexual activity may be restricted during therapy. Vaginal dilator therapy is recommended after treatment to prevent stenosis.
❓ How do I use a vaginal dilator after therapy?
- Start 2 weeks after therapy completion
- Use 3 times a week for 10 minutes per session
- Start with the smallest size and progress gradually
- Use lubricants to ease insertion
- Report persistent pain or bleeding to your doctor
❓ Will I be radioactive after brachytherapy?
No. Once the applicator is removed, your body is no longer radioactive and it is safe to be around others.
🛡️ General Safety & Tips
❓ What symptoms should I report immediately?
- Severe dizziness or fainting
- Persistent vomiting
- Fever > 38°C (100.4°F)
- Prolonged or worsening pain
- Urinary retention or unusual bleeding
❓ Can radiation therapy affect my future pregnancy?
Yes. Pelvic radiation can harm a developing fetus. Always inform your doctor if you are pregnant or planning pregnancy. Consider fertility preservation before therapy.
❓ How should I manage emotional and sexual concerns during therapy?
- Communicate openly with your partner
- Discuss sexual side effects with your care team
- Seek counseling if anxiety, depression, or stress affects intimacy