🧠 Cancer and Psychiatric Disorders: Understanding the Psychological Dimension of Cancer
Discover how cancer affects the human mind and emotions. Learn about cancer psychology, the stages of emotional response, and common psychiatric disorders such as depression, anxiety, and adjustment disorder in oncology patients.
💬 Introduction: The Hidden Burden of Cancer
Cancer is not only a biological disease — it is a psychological and emotional crisis that affects both patients and their families.
Despite remarkable biomedical advances, cancer remains a word associated with death, pain, and suffering. The diagnosis often feels like a sudden catastrophe, forcing individuals to adapt to a new and frightening reality.
When facing cancer, patients must navigate both medical challenges and emotional turmoil. Their ability to cope depends on several factors:
- The type, stage, and prognosis of the disease
- The patient’s psychological resilience and coping style
- Cultural and spiritual beliefs
- The availability of emotional and social support
According to various studies, psychiatric morbidity among cancer patients ranges from 9% to 60%, with most cases arising as a direct psychological reaction to the illness or its treatment. Unfortunately, many of these disorders remain underdiagnosed and undertreated, often due to myths that patients “should” feel bad because they have cancer.
❤️ The Psychological Impact of Cancer
The emotional toll of cancer extends beyond the patient.
Families, caregivers, and even healthcare professionals experience stress, grief, and helplessness.
Patients face the fear of death, uncertainty about their future, and the loss of control over their bodies and lives.
Cancer can affect multiple dimensions of life:
- Physically: pain, fatigue, and loss of body function
- Emotionally: anxiety, sadness, anger, and isolation
- Socially: withdrawal, stigma, or job and financial stress
Even when the prognosis is positive, the diagnosis itself often brings a deep sense of psychological suffering, reshaping how patients see themselves and their world.
🕊️ The Five Stages of Psychological Response to Cancer
Psychiatrist Elisabeth Kübler-Ross, in her pioneering work “On Death and Dying”, identified five emotional stages that terminally ill patients often experience.
While not everyone goes through all of them, these stages remain a cornerstone in understanding cancer psychology.
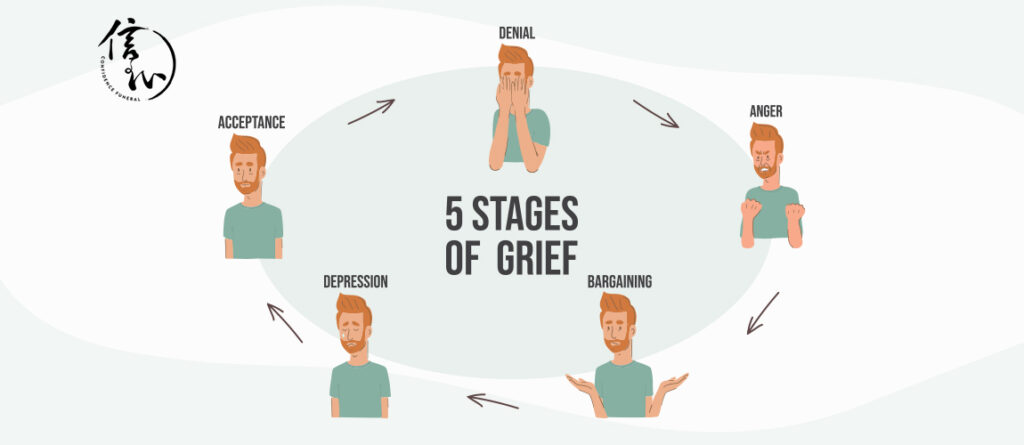
1️⃣ Denial and Isolation (🛑)
The initial response is often shock and disbelief — “This can’t be happening to me.”
Denial acts as a temporary shield, giving patients time to adjust to overwhelming news. It allows emotional recovery before facing the full truth.
2️⃣ Anger (🔥)
When denial fades, anger takes its place — “Why me?”
Patients may feel resentment toward doctors, family, or even fate.
For caregivers, this stage can be challenging, as anger is often projected outward. Understanding that anger is part of the healing process helps maintain empathy and communication.
3️⃣ Bargaining (🤝)
In this phase, patients may attempt to negotiate with themselves, others, or a higher power:
“If I follow every treatment, maybe I’ll get more time.”
Bargaining represents an attempt to regain control and find meaning in uncertainty.
4️⃣ Depression (🌧️)
As reality settles in, sadness and reactive depression emerge.
Patients may mourn the loss of health, independence, or their expected future.
They may withdraw socially, feeling hopeless or fatigued.
Understanding and allowing emotional expression during this phase is essential; false reassurance often deepens despair. Quiet presence, empathy, and touch can communicate more than words.
5️⃣ Acceptance (🌿)
Eventually, many patients reach a calm state of acceptance.
This is not happiness, but rather peace and understanding.
The struggle ends, and a sense of closure begins. Patients may prefer silence, solitude, or meaningful presence rather than conversation.
At this stage, families often need more support than the patient themselves.
🌟 Hope: The Constant Companion
Hope persists through all stages. Even when cure is impossible, hope transforms — from survival, to comfort, to peace.
Doctors and caregivers play a key role in sustaining that hope.
Simple words like “I will continue to care for you and keep you comfortable” preserve dignity and emotional security, even at life’s end.
🧩 Adjustment Disorder in Cancer Patients
Among hospitalized patients, adjustment disorder is one of the most common psychiatric diagnoses.
It occurs when emotional or behavioral symptoms arise in response to a clear stressor — such as a cancer diagnosis or treatment — but are disproportionate to the situation.
🕒 Typical timeline:
Symptoms begin within three months of the stressor and usually resolve within six months after it ends.
In oncology, adjustment disorders often appear as:
- Persistent sadness or worry
- Difficulty adapting to treatment
- Anxiety about the future or prognosis
- Emotional distress related to physical pain or disability
Research indicates that over half of cancer patients experience some form of adjustment difficulty.
This highlights the importance of effective communication between patients and healthcare providers.
According to the World Health Organization (WHO), poor explanations and lack of clarity about diagnosis and treatment options significantly increase psychological distress and patient dissatisfaction.
😟 Anxiety Disorders in Cancer Psychology

Anxiety is a natural reaction to a life-threatening illness — but in cancer, it can become chronic and disabling.
Studies show that anxiety levels are highest among:
- Younger and middle-aged adults
- Women
- Patients undergoing chemotherapy
🔍 Common symptoms:
- Restlessness and tension
- Palpitations or shortness of breath
- Difficulty sleeping
- Excessive worry about recurrence or death
🧪 Research Highlights:
- A study on breast cancer patients found high anxiety and depression levels from diagnosis onward, often lasting over a year.
- Anxiety tends to worsen after surgery, especially in early recovery, and gradually improves later.
- In prostate cancer, anxiety is also common and may be linked to irritability, previous depression, or uncertainty about treatment outcomes.
💊 Management and Treatment:
Treatment must be individualized:
- Benzodiazepines (e.g., lorazepam, alprazolam, diazepam) may help in acute anxiety but require careful use.
- Antidepressants or antipsychotics may be needed in complex cases.
- Non-pharmacological interventions — such as cognitive-behavioral therapy (CBT), relaxation training, and mindfulness — are proven to reduce anxiety and improve quality of life.
🧘♀️ The Role of Psychosocial Interventions
Integrating psychological care into oncology improves not only mental health but also treatment adherence and survival outcomes.
Effective approaches include:
- Psychoeducation – helping patients understand their emotional responses
- Support groups – reducing isolation
- Family therapy – improving communication and coping
- Mind-body therapies – such as meditation, yoga, and guided imagery
These interventions empower patients to reclaim control and maintain dignity during a difficult journey.
🌈 Conclusion: Treating the Mind Alongside the Body
Cancer is not just a battle fought in the body — it’s also a profound psychological journey.
Understanding the principles of cancer psychology allows healthcare providers to address emotional suffering with the same urgency as physical symptoms.
By recognizing psychiatric disorders like depression, anxiety, and adjustment disorder, and by supporting hope, acceptance, and communication, we can transform cancer care into a more humane and holistic experience.
“Healing doesn’t always mean curing. Sometimes, it means helping a person find peace.” 💫
🩺 Psychiatric Symptoms and Treatment Approaches in Cancer Patients
The cancer journey is not only a physical challenge but also an intense psychological experience. Receiving a cancer diagnosis and undergoing treatment can trigger numerous psychiatric symptoms such as mental stress, anxiety, depression, and sleep disturbances. Early recognition and treatment of these psychiatric symptoms improve patients’ quality of life and adherence to treatment.
⚡ Acute Stress Disorder (ASD)
Definition: A rapidly developing, short-term psychiatric disorder following a traumatic event such as a cancer diagnosis.
Duration: Typically lasts less than 30 days.
Symptoms:
- Experiencing fear, helplessness, or horror after real or threatened death
- Dissociative symptoms: numbness, spacing out, depersonalization
- Re-experiencing the trauma: intrusive thoughts, dreams, flashbacks
- Avoidance: steering clear of trauma-related situations or cues
- Hyperarousal: sleep disturbances, irritability, hypervigilance, concentration difficulties
Treatment: Short-term relief can be provided with benzodiazepines.
🧠 Post-Traumatic Stress Disorder (PTSD)
Definition: If acute stress disorder persists beyond 30 days, a diagnosis of PTSD is made.
Types: Acute (<3 months), Chronic (>3 months), Delayed (after 6 months), Recurrent
Prevalence in Cancer Patients: 6–50%, higher in those undergoing chemotherapy
Symptoms: Re-experiencing, avoidance, hyperarousal, numbing
Treatment:
- Medication: SSRIs, sedative antidepressants, anxiolytics, beta-blockers
- Psychotherapy: Cognitive-behavioral therapy (CBT), trauma-focused therapy
😰 Other Anxiety Disorders
Common in cancer patients alongside depression:
- Generalized anxiety: 24%
- Panic disorder: 18%
- PTSD: 30%
Treatment Approach:
- Benzodiazepines (e.g., alprazolam 0.5 mg) are useful in emergencies
- Identify and address triggering factors during diagnostic and treatment processes
💊 Anxiety Due to General Medical Condition
Examples: Carcinoid or endocrine tumors can cause anxiety.
Treatment: Address the underlying medical condition, analgesics, oxygen, or low-dose sedation.
🚬 Substance Withdrawal Syndromes
- Alcohol: Withdrawal symptoms appear within 4–36 hours (sweating, tremor, nausea, agitation)
- Nicotine: Starts 12 hours after the last cigarette and can last several weeks
Treatment: Benzodiazepines, nicotine replacement, behavioral programs
😔 Depression
Prevalence: Major depression occurs in 10–25% of cancer patients, average 22%
Symptoms:
- Depressed mood
- Loss of interest or pleasure
- Appetite and weight changes
- Sleep disturbances
- Psychomotor changes
- Fatigue
- Guilt
- Concentration difficulties
- Thoughts of death or suicide
Treatment:
- Psychosocial: Support groups, CBT, psychoeducation
- Pharmacological: SSRIs, SNRIs, mirtazapine, low-dose antidepressants
💤 Sleep Disorders
Prevalence: 50% of cancer patients, more common in women
Causes: Diagnosis stress, treatment side effects, iatrogenic effects
Consequences: Fatigue, cognitive impairment, reduced quality of life
Treatment: Hypnotics, sleep hygiene, relaxation therapy, behavioral strategies
🧪 Fatigue
Definition: Fatigue that does not improve with rest, affecting physical and mental functioning
Prevalence: Post-breast cancer 91%, Hodgkin lymphoma 26%
Causes: Cytokine dysregulation, anemia, dyspnea, chemotherapy, drug side effects
Treatment: Exercise, psychotherapy, massage therapy, epoetin alfa
🧩 Organic Psychiatric Disorders (Delirium)
Prevalence: 14–55% in hospitalized patients, 90% in the final weeks of life
Types: Hyperactive, hypoactive, mixed
Symptoms: Mood changes, hallucinations, disorientation, agitation
Treatment: Haloperidol, olanzapine, risperidone, lorazepam; address underlying causes
⚠️ Suicide Risk
Increased Risk: Early post-diagnosis period, advanced disease, young age, radiotherapy
Symptoms: Low self-esteem, depression, chronic pain, social isolation
Prevention: Psychological support, management of depression and pain, family and social support
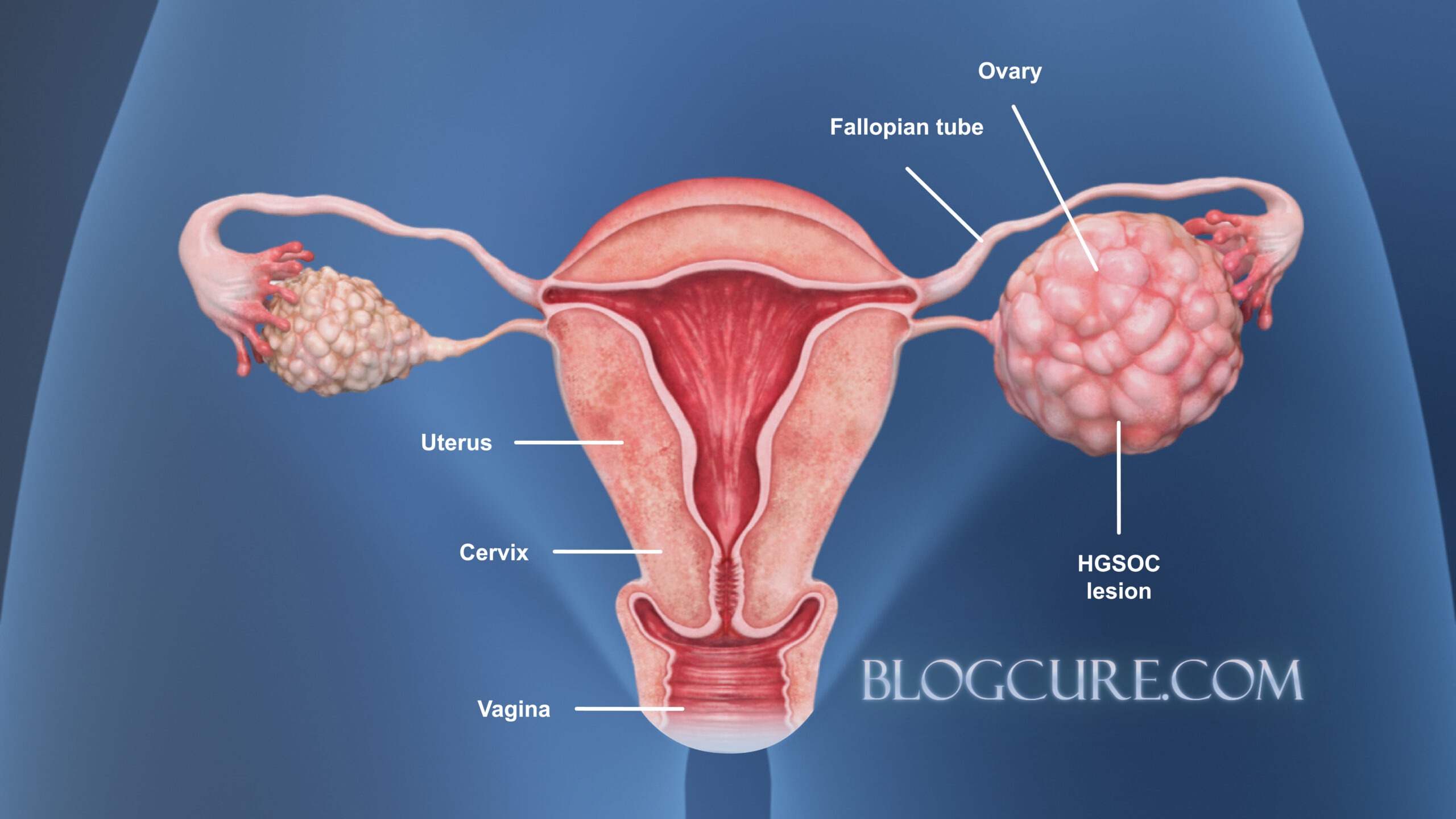
❤️ Sexual Dysfunction

Causes: Surgery, chemotherapy, hormone therapy, radiotherapy, psychological effects
- Women: Postmenopausal symptoms after breast cancer, vaginal dryness
- Men: Erectile dysfunction and ejaculation problems after prostate or testicular cancer
Treatment: Counseling, lubricants, phosphodiesterase-5 inhibitors (e.g., sildenafil)
📌 Psychiatric Disorders Related to Cancer Treatment
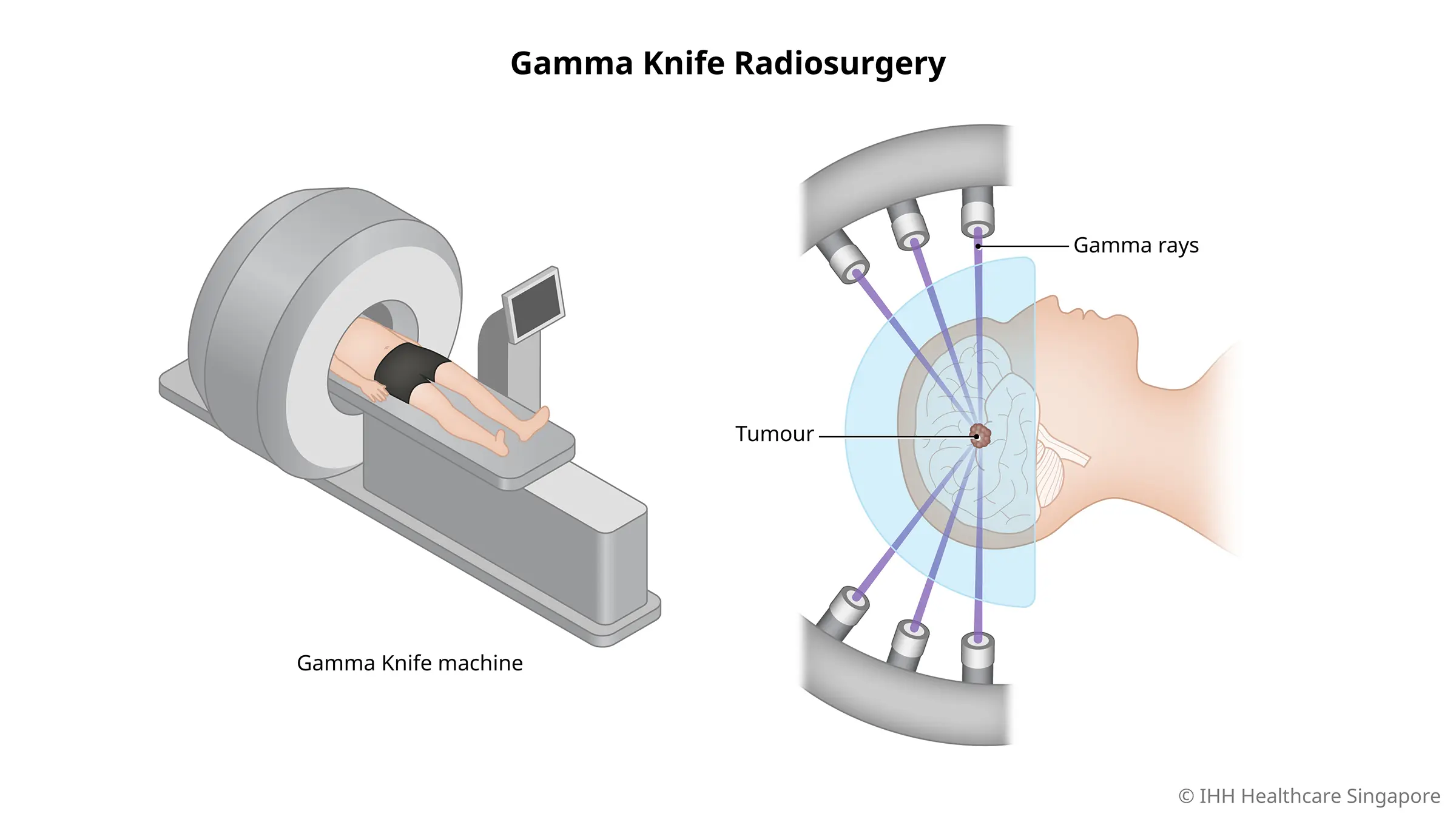
- Radiotherapy: Encephalopathy and neuropsychiatric disorders
- Medications: Steroids, interferon, chemotherapy agents
Consequences: Sleep disturbances, personality changes, memory impairment
Psychiatric Condition Definition / Description Prevalence in Cancer Patients Key Symptoms Treatment Approaches Icon Suggestion
Acute Stress Disorder (ASD) Short-term psychiatric reaction after a traumatic event (e.g., cancer diagnosis) Less than 30 days duration Fear, helplessness, dissociation, flashbacks, avoidance, hyperarousal Short-term benzodiazepines for relief ⚡
Post-Traumatic Stress Disorder (PTSD) Persistent stress symptoms >30 days after trauma 6–50%; higher in chemotherapy patients Re-experiencing, avoidance, hyperarousal, emotional numbing SSRIs, sedative antidepressants, anxiolytics, beta-blockers, CBT, trauma-focused therapy 🧠
Generalized Anxiety / Panic Disorder Anxiety disorders co-occurring with cancer GAD 24%, Panic 18%, PTSD 30% Excessive worry, panic attacks, hyperarousal Emergency benzodiazepines, trigger management 😰
Anxiety due to Medical Condition Anxiety caused by tumors or systemic illness Varies Tumor-related stress, agitation, somatic anxiety Treat underlying medical condition, analgesics, oxygen, low-dose sedation 💊
Substance Withdrawal Alcohol or nicotine withdrawal Alcohol: 4–36 hrs, Nicotine: 12 hrs Sweating, tremor, nausea, agitation Benzodiazepines, nicotine replacement, behavioral programs 🚬
Depression Major depressive episode or persistent depressive symptoms Major 10–25%, average 22% Low mood, anhedonia, sleep/appetite changes, fatigue, guilt, suicidal thoughts Psychosocial support, CBT, psychoeducation, SSRIs/SNRIs/mirtazapine 😔
Sleep Disorders Insomnia or fragmented sleep related to diagnosis or treatment 50%, more common in women Difficulty falling/staying asleep, fatigue, cognitive impairment Hypnotics, sleep hygiene, relaxation therapy, behavioral strategies 🌙
Fatigue Persistent tiredness not relieved by rest Post-breast cancer 91%, Hodgkin lymphoma 26% Physical & mental exhaustion, decreased functioning Exercise, psychotherapy, massage therapy, epoetin alfa 🏃♂️
Delirium / Organic Psychiatric Disorders Acute cognitive disturbances due to illness or treatment 14–55% hospitalized, 90% end-of-life Mood swings, hallucinations, disorientation, agitation Haloperidol, olanzapine, risperidone, lorazepam, treat underlying cause 🌀
Suicide Risk Elevated risk during cancer treatment Higher in early post-diagnosis, advanced disease, young patients Low self-esteem, depression, chronic pain, social isolation Psychological support, depression & pain management, family support ⚠️
Sexual Dysfunction Treatment-induced sexual problems Women: postmenopausal / vaginal dryness; Men: ED, ejaculatory issues Loss of libido, erectile problems, vaginal dryness Counseling, lubricants, PDE-5 inhibitors (sildenafil) ❤️
Treatment-Induced Psychiatric Disorders Side effects of chemotherapy, radiotherapy, steroids Variable Sleep disturbances, personality change, memory issues Symptomatic management, medication adjustment, psychosocial support 💉
Frequently Asked Questions (FAQ) – Psychiatric Conditions in Cancer Patients
1. ⚡ What is Acute Stress Disorder (ASD) in cancer patients?
Acute Stress Disorder is a short-term psychiatric reaction to a traumatic event, such as receiving a cancer diagnosis. Symptoms include fear, helplessness, dissociation, flashbacks, avoidance, and hyperarousal. It usually lasts less than 30 days. Short-term use of benzodiazepines can help relieve symptoms.
2. 🧠 How common is PTSD among cancer patients?
Post-Traumatic Stress Disorder (PTSD) affects 6–50% of cancer patients, with higher rates in those undergoing chemotherapy. Key symptoms include re-experiencing trauma, avoidance, hyperarousal, and emotional numbness. Treatments include SSRIs, sedative antidepressants, anxiolytics, beta-blockers, cognitive behavioral therapy (CBT), and trauma-focused therapy.
3. 😰 What are the signs of anxiety in cancer patients?
Cancer patients may experience Generalized Anxiety Disorder (GAD) or Panic Disorder, characterized by excessive worry, panic attacks, and hyperarousal. GAD occurs in 24% and Panic Disorder in 18% of patients. Emergency benzodiazepines and trigger management are commonly used treatments.
4. 💊 Can cancer itself cause anxiety?
Yes. Anxiety due to medical conditions can result from tumors or systemic illness. Patients may feel tumor-related stress, agitation, or somatic anxiety. Managing the underlying condition along with analgesics, oxygen, and low-dose sedation can help.
5. 🚬 How does substance withdrawal affect cancer patients?
Alcohol or nicotine withdrawal may occur in hospitalized patients. Symptoms include sweating, tremor, nausea, and agitation. Treatment may involve benzodiazepines, nicotine replacement therapy, and behavioral programs.
6. 😔 How common is depression in cancer patients?
Depression affects 10–25% of patients as a major depressive episode and about 22% overall. Symptoms include low mood, anhedonia, changes in sleep/appetite, fatigue, guilt, and suicidal thoughts. Treatments include psychosocial support, CBT, psychoeducation, and medications like SSRIs, SNRIs, or mirtazapine.
7. 🌙 Why do cancer patients experience sleep disorders?
Up to 50% of cancer patients, especially women, suffer from sleep disorders due to diagnosis or treatment. Symptoms include difficulty falling or staying asleep, fatigue, and cognitive impairment. Treatment options include hypnotics, sleep hygiene, relaxation therapy, and behavioral strategies.
8. 🏃♂️ What causes fatigue in cancer patients?
Fatigue is persistent tiredness not relieved by rest. It affects up to 91% of breast cancer patients post-treatment and 26% of Hodgkin lymphoma patients. Symptoms include physical and mental exhaustion and decreased functioning. Management includes exercise, psychotherapy, massage therapy, and epoetin alfa.
9. 🌀 What is delirium, and how is it managed in cancer patients?
Delirium is an acute cognitive disturbance due to illness or treatment, occurring in 14–55% of hospitalized patients and up to 90% at the end of life. Symptoms include mood swings, hallucinations, disorientation, and agitation. Treatments include haloperidol, olanzapine, risperidone, lorazepam, and addressing underlying causes.
10. ⚠️ Are cancer patients at higher risk of suicide?
Yes. Suicide risk is higher in the early post-diagnosis period, in advanced disease, and in younger patients. Risk factors include low self-esteem, depression, chronic pain, and social isolation. Prevention strategies include psychological support, depression and pain management, and family support.
11. ❤️ How does cancer treatment affect sexual function?
Treatment-induced sexual dysfunction is common. Women may experience postmenopausal symptoms or vaginal dryness, while men may experience erectile dysfunction or ejaculatory issues. Management includes counseling, lubricants, and PDE-5 inhibitors like sildenafil.
12. 💉 Can cancer treatments cause psychiatric symptoms?
Yes. Chemotherapy, radiotherapy, and steroid treatments may cause sleep disturbances, personality changes, or memory issues. Symptomatic management, medication adjustments, and psychosocial support are recommended.